In emergency medicine, a lucid interval is a temporary improvement in a patient's condition after a traumatic brain injury, after which the condition deteriorates. A lucid interval is especially indicative of an epidural hematoma. An estimated 20 to 50% of patients with epidural hematoma experience such a lucid interval.

Hyperekplexia is a very rare neurologic disorder, classically characterised by a pronounced startle responses to tactile or acoustic stimuli and an ensuing period of hypertonia. The hypertonia may be predominantly truncal, attenuated during sleep, or less prominent after one year of age.
Generalized epilepsy with febrile seizures plus (GEFS+) is a syndromic autosomal dominant disorder where affected individuals can exhibit numerous epilepsy phenotypes. GEFS+ can persist beyond early childhood. GEFS+ is also now believed to encompass three other epilepsy disorders: severe myoclonic epilepsy of infancy (SMEI), which is also known as Dravet's syndrome, borderline SMEI (SMEB), and intractable epilepsy of childhood (IEC). There are at least six types of GEFS+, delineated by their causative gene. Known causative gene mutations are in the sodium channel α subunit genes SCN1A, an associated β subunit SCN1B, and in a GABAA receptor γ subunit gene, in GABRG2 and there is another gene related with calcium channel the PCDH19 which is also known as Epilepsy Female with Mental Retardation. Penetrance for this disorder is estimated at 60%.
Benign familial neonatal seizures (BFNS), also referred to as benign familial neonatal epilepsy (BFNE), is a rare autosomal dominant inherited form of seizures. This condition manifests in newborns as brief and frequent episodes of tonic-clonic seizures with asymptomatic periods in between. Characteristically, seizure activity spontaneously ends during infancy and does not affect childhood development. However, some studies have reported that a minority of children with BFNS consequently develop intellectual disability. Additionally, BFNS increases lifetime susceptibility to seizures as approximately 14% of those afflicted go on to develop epilepsy later in life. There are three known genetic causes of BFNE, two being the voltage-gated potassium channels KCNQ2 (BFNC1) and KCNQ3 (BFNC2) and the third being a chromosomal inversion (BFNC3). There is no obvious correlation between most of the known mutations and clinical variability seen in BFNE.

Hemiplegic migraine is a type of migraine headache characterized by motor weakness affecting only one side of the body, accompanied by aura. There is often an impairment in vision, speech, or sensation. It can run in the family, called familial hemiplegic migraine, or in a single individual, called sporadic hemiplegic migraine. The symptoms can be similar to a stroke, and may be precipitated by minor head trauma. People with FHM are advised to avoid activities that may trigger their attacks.

Sporadic hemiplegic migraine (SHM) is a form of hemiplegic migraine headache isolated cases of which are observed. It is a rare disease. It is considered to be a separate type of migraine.

Spinocerebellar ataxia type 6 (SCA6) is a rare, late-onset, autosomal dominant disorder, which, like other types of SCA, is characterized by dysarthria, oculomotor disorders, peripheral neuropathy, and ataxia of the gait, stance, and limbs due to cerebellar dysfunction. Unlike other types, SCA 6 is not fatal. This cerebellar function is permanent and progressive, differentiating it from episodic ataxia type 2 (EA2) where said dysfunction is episodic. In some SCA6 families, some members show these classic signs of SCA6 while others show signs more similar to EA2, suggesting that there is some phenotypic overlap between the two disorders. SCA6 is caused by mutations in CACNA1A, a gene encoding a calcium channel α subunit. These mutations tend to be trinucleotide repeats of CAG, leading to the production of mutant proteins containing stretches of 20 or more consecutive glutamine residues; these proteins have an increased tendency to form intracellular agglomerations. Unlike many other polyglutamine expansion disorders expansion length is not a determining factor for the age that symptoms present.
Episodic ataxia (EA) is an autosomal dominant disorder characterized by sporadic bouts of ataxia with or without myokymia. There are seven types recognized but the majority are due to two recognized entities. Ataxia can be provoked by psychological stress or startle, or heavy exertion, including exercise. Symptoms can first appear in infancy. There are at least six loci for EA, of which 4 are known genes. Some patients with EA also have migraine or progressive cerebellar degenerative disorders, symptomatic of either familial hemiplegic migraine or spinocerebellar ataxia. Some patients respond to acetazolamide though others do not.

Spinocerebellar ataxia type 13 (SCA13) is a rare autosomal dominant disorder, which, like other types of SCA, is characterized by dysarthria, nystagmus, and ataxia of gait, stance and the limbs due to cerebellar dysfunction. Patients with SCA13 also tend to present with epilepsy, an inability to run, and increased reflexes. This cerebellar dysfunction is permanent and progressive. SCA13 is caused by mutations in KCNC3, a gene encoding a voltage-gated potassium channel KV3.3. There are two known mutations in this gene causative for SCA13. Unlike many other types of SCA, these are not polyglutamine expansions but, rather, point mutations resulting in channels with no current or altered kinetics.
The R-type calcium channel is a type of voltage-dependent calcium channel. Like the others of this class, the α1 subunit forms the pore through which calcium enters the cell and determines most of the channel's properties. This α1 subunit is also known as the calcium channel, voltage-dependent, R type, alpha 1E subunit (CACNA1E) or Cav2.3 which in humans is encoded by the CACNA1E gene. They are strongly expressed in cortex, hippocampus, striatum, amygdala and interpeduncular nucleus.
The P-type calcium channel is a type of voltage-dependent calcium channel. Similar to many other high-voltage-gated calcium channels, the α1 subunit determines most of the channel's properties. The 'P' signifies cerebellar Purkinje cells, referring to the channel's initial site of discovery. P-type calcium channels play a similar role to the N-type calcium channel in neurotransmitter release at the presynaptic terminal and in neuronal integration in many neuronal types.

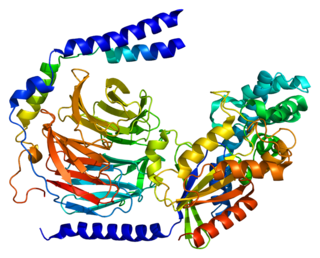
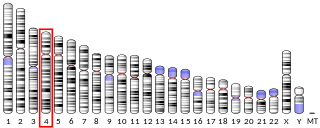
Cav2.1, also called the P/Q voltage-dependent calcium channel, is a calcium channel found mainly in the brain. Specifically, it is found on the presynaptic terminals of neurons in the brain and cerebellum. Cav2.1 plays an important role in controlling the release of neurotransmitters between neurons. It is composed of multiple subunits, including alpha-1, beta, alpha-2/delta, and gamma subunits. The alpha-1 subunit is the pore-forming subunit, meaning that the calcium ions flow through it. Different kinds of calcium channels have different isoforms (versions) of the alpha-1 subunit. Cav2.1 has the alpha-1A subunit, which is encoded by the CACNA1A gene. Mutations in CACNA1A have been associated with various neurologic disorders, including familial hemiplegic migraine, episodic ataxia type 2, and spinocerebellar ataxia type 6.

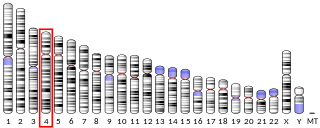
Sodium channel protein type 1 subunit alpha (SCN1A), is a protein which in humans is encoded by the SCN1A gene.
Sodium/potassium-transporting ATPase subunit alpha-2 is a protein which in humans is encoded by the ATP1A2 gene.
Guanine nucleotide-binding protein G(I)/G(S)/G(O) subunit gamma-2 is a protein that in humans is encoded by the GNG2 gene.

Sodium/potassium-transporting ATPase subunit alpha-3 is an enzyme that in humans is encoded by the ATP1A3 gene.
Glutamate receptor, ionotropic, delta 2, also known as GluD2, GluRδ2, or δ2, is a protein that in humans is encoded by the GRID2 gene. This protein together with GluD1 belongs to the delta receptor subtype of ionotropic glutamate receptors. They possess 14–24% sequence homology with AMPA, kainate, and NMDA subunits, but, despite their name, do not actually bind glutamate or various other glutamate agonists.

Proline-rich transmembrane protein 2 is a protein that in humans is encoded by the PRRT2 gene.
Migraine is often hereditary. It is estimated that 60% of migraine cases are caused by genetics. The role of natural selection in the development of migraines is not known. Fitness-impairing disorders, including migraines, tend to disappear as a result of natural selection, and their frequency decreases to near the rate of spontaneous mutation. However, it is estimated that migraines affect 15-20% of the population and is increasing. This could suggest that a central nervous system (CNS) susceptible to severe, intermittent headache has been linked to an important survival or reproductive advantage. Five possible evolutionary explanations exist: i) migraine as a defence mechanism, ii) migraine as a result of conflicts with other organisms, iii) migraine as a result of novel environmental factors, iv) migraine as a compromise between genetic harms and benefits, and v) headache as a design constraint. These considerations allow the treatment and prevention of migraine to be approached from an evolutionary medicine perspective.
A heme transporter is a protein that delivers heme to the various parts of a biological cell that require it.