Related Research Articles

Migraine is a genetically-influenced complex neurological disorder characterized by episodes of moderate-to-severe headache, most often unilateral and generally associated with nausea and light and sound sensitivity. Other characterizing symptoms may include nausea, vomiting, cognitive dysfunction, allodynia, and dizziness. Exacerbation of headache symptoms during physical activity is another distinguishing feature.

A seizure is a period of symptoms due to abnormally excessive or synchronous neuronal activity in the brain. Outward effects vary from uncontrolled shaking movements involving much of the body with loss of consciousness, to shaking movements involving only part of the body with variable levels of consciousness, to a subtle momentary loss of awareness. These episodes usually last less than two minutes and it takes some time to return to normal. Loss of bladder control may occur.

An aura is a perceptual disturbance experienced by some with epilepsy or migraine. An epileptic aura is actually a minor seizure.
Psychogenic non-epileptic seizures (PNES), also referred to as pseudoseizures, non-epileptic attack disorder (NEAD), functional seizures, or dissociative seizures, are episodes resembling an epileptic seizure but without the characteristic electrical discharges associated with epilepsy. PNES fall under the category of disorders known as functional neurological disorders (FND) and are typically treated by psychologists or psychiatrists.
Frontal lobe epilepsy (FLE) is a neurological disorder that is characterized by brief, recurring seizures arising in the frontal lobes of the brain, that often occur during sleep. It is the second most common type of epilepsy after temporal lobe epilepsy (TLE), and is related to the temporal form in that both forms are characterized by partial (focal) seizures.
Myoclonic epilepsy refers to a family of epilepsies that present with myoclonus. When myoclonic jerks are occasionally associated with abnormal brain wave activity, it can be categorized as myoclonic seizure. If the abnormal brain wave activity is persistent and results from ongoing seizures, then a diagnosis of myoclonic epilepsy may be considered.
The postictal state is the altered state of consciousness after an epileptic seizure. It usually lasts between 5 and 30 minutes, but sometimes longer in the case of larger or more severe seizures, and is characterized by drowsiness, confusion, nausea, hypertension, headache or migraine, and other disorienting symptoms.
Abdominal epilepsy is a rare condition most frequently found in children, consisting of gastrointestinal disturbances caused by epileptiform seizure activity. Though a few cases of it have been reported in adults too. It has been described as a type of temporal lobe epilepsy. Responsiveness to anticonvulsants can aid in the diagnosis. Distinguishing features of abdominal epilepsy include (1) Abnormal laboratory, radiographic, and endoscopic findings revealing paroxysmal GI manifestations of unknown origin (2) CNS symptoms (3) Abnormal EEG. Most published medical literature dealing with abdominal epilepsy is in the form of individual case reports. A 2005 review article found a total of 36 cases described in the medical literature.
Todd's paresis is focal weakness in a part or all of the body after a seizure. This weakness typically affects the limbs and is localized to either the left or right side of the body. It usually subsides completely within 48 hours. Todd's paresis may also affect speech, eye position (gaze), or vision.

A generalized tonic–clonic seizure, commonly known as a grand mal seizure or GTCS, is a type of generalized seizure that produces bilateral, convulsive tonic and clonic muscle contractions. Tonic–clonic seizures are the seizure type most commonly associated with epilepsy and seizures in general and the most common seizure associated with metabolic imbalances. It is a misconception that they are the sole type of seizure, as they are the main seizure type in approximately 10% of those with epilepsy.
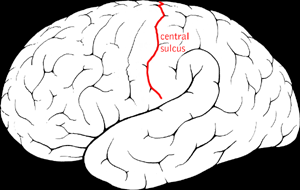
Benign Rolandic epilepsy or self-limited epilepsy with centrotemporal spikes is the most common epilepsy syndrome in childhood. Most children will outgrow the syndrome, hence the label benign. The seizures, sometimes referred to as sylvian seizures, start around the central sulcus of the brain.
Panayiotopoulos syndrome is a common idiopathic childhood-related seizure disorder that occurs exclusively in otherwise normal children and manifests mainly with autonomic epileptic seizures and autonomic status epilepticus. An expert consensus has defined Panayiotopoulos syndrome as "a benign age-related focal seizure disorder occurring in early and mid-childhood. It is characterized by seizures, often prolonged, with predominantly autonomic symptoms, and by an EEG [electroencephalogram] that shows shifting and/or multiple foci, often with occipital predominance."
New daily persistent headache (NDPH) is a primary headache syndrome which can mimic chronic migraine and chronic tension-type headache. The headache is daily and unremitting from very soon after onset, usually in a person who does not have a history of a primary headache disorder. The pain can be intermittent, but lasts more than 3 months. Headache onset is abrupt and people often remember the date, circumstance and, occasionally, the time of headache onset. One retrospective study stated that over 80% of patients could state the exact date their headache began.
Migralepsy is a rare condition in which a migraine is followed, within an hour period, by an epileptic seizure. Because of the similarities in signs, symptoms, and treatments of both conditions, such as the neurological basis, the psychological issues, and the autonomic distress that is created from them, they individually increase the likelihood of causing the other. However, also because of the sameness, they are often misdiagnosed for each other, as migralepsy rarely occurs.
Abdominal aura, also known as visceral aura and epigastric aura, is a type of somatosensory aura that typically manifests as abdominal discomfort in the form of nausea, malaise, hunger, or pain. Abdominal aura is typically associated with epilepsy, especially temporal lobe epilepsy, and it can also be used in the context of migraine. The term is used to distinguish it from other types of somatosensory aura, notably visual disturbances and paraesthesia. The abdominal aura can be classified as a somatic hallucination. Pathophysiologically, the abdominal aura is associated with aberrant neuronal discharges in sensory cortical areas representing the abdominal viscera.
Forced Normalization (FN) is a psychiatric phenomenon in which a long term episodic epilepsy or migraine disorder is treated, and, although the electroencephalogram (EEG) appears to have stabilized, acute behavioral, mood, and psychological disturbances begin to manifest. If, or when, treatment for the disorder is halted, the disturbances go away, but the episodic spikes on the EEG reappear. H. Landolt coined the term 'Forced Normalization' in 1953 in response to a change he witnessed in epileptic EEGs, which monitor electrical activity in the brain. These changes were followed by abrupt behavioral changes in the patient. Landolt concluded that forced normalization is "the phenomenon characterized by the fact that, with the occurrence of psychotic states, the electroencephalography becomes more normal or entirely normal, as compared with previous and subsequent EEG findings." Forced normalization, as described by Landolt, was therefore an electrophysiological phenomenon with the electroencephalograph at its helm.
Idiopathic childhood occipital epilepsy of Gastaut (ICOE-G) is a pure but rare form of idiopathic occipital epilepsy that affects otherwise normal children and adolescents. It is classified amongst benign idiopathic childhood focal epilepsies such as rolandic epilepsy and Panayiotopoulos syndrome.

Occipital epilepsy is a neurological disorder that arises from excessive neural activity in the occipital lobe of the brain that may or may not be symptomatic. Occipital lobe epilepsy is fairly rare, and may sometimes be misdiagnosed as migraine when symptomatic. Epileptic seizures are the result of synchronized neural activity that is excessive, and may stem from a failure of inhibitory neurons to regulate properly.
A migrainous infarction is a rare type of ischaemic stroke which occurs in correspondence with migraine aura symptoms. Symptoms include headaches, visual disturbances, strange sensations and dysphasia, all of which gradually worsen causing neurological changes which ultimately increase the risk of an ischaemic stroke. Typically, women under the age of 45 who experience migraine with aura (MA) are at the greatest risk for developing migrainous infarction, especially when combined with smoking and use of oral contraceptives.
Menstrual migraine is the term used to describe both true menstrual migraines and menstrually related migraines. About 7%–14% of women have migraines only at the time of menstruation. These are called true menstrual migraines. Most female migraineurs experience migraine attacks throughout the menstruation cycle with an increased number perimenstrually, these are referred to as menstrually related or menstrually triggered migraine.
References
- ↑ Piccioli M, Parisi P, Tisei P, Villa MP, Buttinelli C, Kasteleijn-Nolst Trenité DG (February 2009). "Ictal headache and visual sensitivity". Cephalalgia. 29 (2): 194–203. doi:10.1111/j.1468-2982.2008.01707.x. PMID 18823360. S2CID 7911641.
- 1 2 Parisi P, Verrotti A, Costa P, Striano P, Zanus C, Carrozzi M, Raucci U, Villa MP, Belcastro V (September 2015). "Diagnostic criteria currently proposed for "ictal epileptic headache": perspectives on strengths, weaknesses and pitfalls". Seizure. 31 (2): 56–63. doi: 10.1016/j.seizure.2015.07.005 . PMID 26362378. S2CID 18739241.
- 1 2 3 4 5 Cianchetti C, Dainese F, Ledda MG, Avanzini G (November 2017). "Epileptic headache: a rare form of painful seizure". Seizure. 52: 169–175. doi: 10.1016/j.seizure.2017.10.010 . PMID 29054038.
- 1 2 3 Headache Classification Committee of the International Headache Society (IHS) (January 2018). "The International Classification of Headache Disorders, 3rd edition". Cephalalgia. 38 (1): 1–211. doi: 10.1177/0333102417738202 . PMID 29368949. S2CID 45901670.
- 1 2 3 Cianchetti C, Avanzini G, Dainese F, Guidetti V (June 2017). "The complex interrelations between two paroxysmal disorders: headache and epilepsy". Neurological Sciences. 38 (6): 941–948. doi:10.1007/s10072-017-2926-5. PMID 28341968. S2CID 4228459.
- ↑ Ekstein D, Schachter SC (October 2010). "Postictal headache". Epilepsy & Behavior. 19 (2): 151–155. doi:10.1016/j.yebeh.2010.06.023. PMID 20829119. S2CID 44473900.
- ↑ Hwang ST, Goodman T, Stevens SJ (September 2019). "Painful seizures: a review of epileptic ictal pain". Curr. Pain Headache Rep. 23 (11): 169–175. doi:10.1007/s11916-019-0825-6. PMID 31506775. S2CID 202160283.
- ↑ Cianchetti C, Pruna D, Porcu L, Peltz MT, Ledda MG (March 2013). "Pure epileptic headache and related manifestations: a video-EEG report and discussion of terminology". Epileptic Disorders. 15 (1): 84–92. doi: 10.1684/epd.2013.0552 . PMID 23518661.
- ↑ Belcastro V, Striano P, Pierguidi L, Calabresi P, Tambasco N (January 2011). "Ictal epileptic headache mimicking status migrainosus: EEG and DWI-MRI findings". Headache. 51 (1): 160–162. doi:10.1111/j.1526-4610.2010.01709.x. PMID 20553328. S2CID 24924404.
- ↑ Mainieri G, Cevoli S, Giannini G, Zummo L, Leta C, Broli M, Ferri L, Santucci M, Posar A, Avoni P, Cortelli P, Tinuper P, Bisulli F (August 2015). "Headache in epilepsy: prevalence and clinical features". J. Headache Pain. 16: 556. doi: 10.1186/s10194-015-0556-y . PMC 4540713 . PMID 26245188.