Related Research Articles

The greater occipital nerve is a nerve of the head. It is a spinal nerve, specifically the medial branch of the dorsal primary ramus of cervical spinal nerve 2. It arises from between the first and second cervical vertebrae, ascends, and then passes through the semispinalis muscle. It ascends further to supply the skin along the posterior part of the scalp to the vertex. It supplies sensation to the scalp at the top of the head, over the ear and over the parotid glands.

A bone tumor is an abnormal growth of tissue in bone, traditionally classified as noncancerous (benign) or cancerous (malignant). Cancerous bone tumors usually originate from a cancer in another part of the body such as from lung, breast, thyroid, kidney and prostate. There may be a lump, pain, or neurological signs from pressure. A bone tumor might present with a pathologic fracture. Other symptoms may include fatigue, fever, weight loss, anemia and nausea. Sometimes there are no symptoms and the tumour is found when investigating another problem.

Cluster headache (CH) is a neurological disorder characterized by recurrent severe headaches on one side of the head, typically around the eye(s). There is often accompanying eye watering, nasal congestion, or swelling around the eye on the affected side. These symptoms typically last 15 minutes to 3 hours. Attacks often occur in clusters which typically last for weeks or months and occasionally more than a year.

Trigeminal neuralgia, also called Fothergill disease, tic douloureux, or trifacial neuralgia is a long-term pain disorder that affects the trigeminal nerve, the nerve responsible for sensation in the face and motor functions such as biting and chewing. It is a form of neuropathic pain. There are two main types: typical and atypical trigeminal neuralgia. The typical form results in episodes of severe, sudden, shock-like pain in one side of the face that lasts for seconds to a few minutes. Groups of these episodes can occur over a few hours. The atypical form results in a constant burning pain that is less severe. Episodes may be triggered by any touch to the face. Both forms may occur in the same person. It is regarded as one of the most painful disorders known to medicine, and often results in depression and suicide.
Postherpetic neuralgia (PHN) is neuropathic pain that occurs due to damage to a peripheral nerve caused by the reactivation of the varicella zoster virus. PHN is defined as pain in a dermatomal distribution that lasts for at least 90 days after an outbreak of herpes zoster. Several types of pain may occur with PHN including continuous burning pain, episodes of severe shooting or electric-like pain, and a heightened sensitivity to gentle touch which would not otherwise cause pain or to painful stimuli. Abnormal sensations and itching may also occur.
Neuralgia is pain in the distribution of a nerve or nerves, as in intercostal neuralgia, trigeminal neuralgia, and glossopharyngeal neuralgia.
Chronic paroxysmal hemicrania (CPH) is a severe debilitating unilateral headache usually affecting the area around the eye. It normally consists of multiple severe, yet short, headache attacks affecting only one side of the cranium. It is more commonly diagnosed in women than in men, but, unlike a migraine, has no neurological symptoms associated with it. CPH headaches are treated through the use of non-steroidal anti-inflammatory drugs, with indomethacin found to be usually effective in eliminating symptoms.
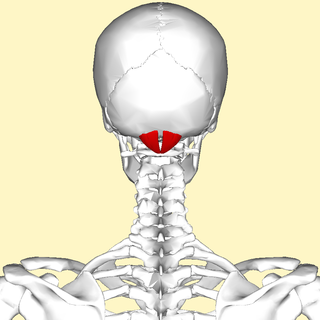
The rectus capitis posterior minor is a muscle in the upper back part of the neck. It is one of the suboccipital muscles. Its inferior attachment is at the posterior arch of atlas; its superior attachment is onto the occipital bone at and below the inferior nuchal line. The muscle is innervated by the suboccipital nerve. The muscle acts as a weak extensor of the head.

Radiofrequency ablation (RFA), also called fulguration, is a medical procedure in which part of the electrical conduction system of the heart, tumor or other dysfunctional tissue is ablated using the heat generated from medium frequency alternating current. RFA is generally conducted in the outpatient setting, using either local anesthetics or twilight anesthesia. When it is delivered via catheter, it is called radiofrequency catheter ablation.
A neurectomy, or nerve resection is a neurosurgical procedure in which a peripheral nerve is cut or removed to alleviate neuropathic pain or permanently disable some function of a nerve. The nerve is not intended to grow back. For chronic pain it may be an alternative to a failed nerve decompression when the target nerve has no motor function and numbness is acceptable. Neurectomies have also been used to permanently block autonomic function, and special sensory function not related to pain.
Geniculate ganglionitis or geniculate neuralgia (GN), also called nervus intermedius neuralgia, Ramsay Hunt syndrome, or Hunt's neuralgia, is a rare disorder characterized by severe paroxysmal neuralgic pain deep in the ear, that may spread to the ear canal, outer ear, mastoid or eye regions. GN may also occur in combination with trigeminal or glossopharyngeal neuralgia.
Migraine surgery is a surgical operation undertaken with the goal of reducing or preventing migraines. Migraine surgery most often refers to surgical nerve decompression of one or several nerves in the head and neck which have been shown to trigger migraine symptoms in many migraine sufferers. Following the development of nerve decompression techniques for the relief of migraine pain in the year 2000, these procedures have been extensively studied and shown to be effective in appropriate candidates. The nerves that are most often addressed in migraine surgery are found outside of the skull, in the face and neck, and include the supra-orbital and supra-trochlear nerves in the forehead, the zygomaticotemporal nerve and auriculotemporal nerves in the temple region, and the greater occipital, lesser occipital, and third occipital nerves in the back of the neck. Nerve impingement in the nasal cavity has additionally been shown to be a trigger of migraine symptoms.

Atypical trigeminal neuralgia (ATN), or type 2 trigeminal neuralgia, is a form of trigeminal neuralgia, a disorder of the fifth cranial nerve. This form of nerve pain is difficult to diagnose, as it is rare and the symptoms overlap with several other disorders. The symptoms can occur in addition to having migraine headache, or can be mistaken for migraine alone, or dental problems such as temporomandibular joint disorder or musculoskeletal issues. ATN can have a wide range of symptoms and the pain can fluctuate in intensity from mild aching to a crushing or burning sensation, and also to the extreme pain experienced with the more common trigeminal neuralgia.

Cranial nerve disease is an impaired functioning of one of the twelve cranial nerves. Although it could theoretically be considered a mononeuropathy, it is not considered as such under MeSH.

Nerve compression syndrome, or compression neuropathy, or nerve entrapment syndrome, is a medical condition caused by chronic, direct pressure on a peripheral nerve. It is known colloquially as a trapped nerve, though this may also refer to nerve root compression. Its symptoms include pain, tingling, numbness and muscle weakness. The symptoms affect just one particular part of the body, depending on which nerve is affected. The diagnosis is largely clinical and can be confirmed with diagnostic nerve blocks. Occasionally imaging and electrophysiology studies aid in the diagnosis. Timely diagnosis is important as untreated chronic nerve compression may cause permanent damage. A surgical nerve decompression can relieve pressure on the nerve but cannot always reverse the physiological changes that occurred before treatment. Nerve injury by a single episode of physical trauma is in one sense an acute compression neuropathy but is not usually included under this heading, as chronic compression takes a unique pathophysiological course.
Atypical facial pain (AFP) is a type of chronic facial pain which does not fulfill any other diagnosis. There is no consensus as to a globally accepted definition, and there is even controversy as to whether the term should be continued to be used. Both the International Headache Society (IHS) and the International Association for the Study of Pain (IASP) have adopted the term persistent idiopathic facial pain (PIFP) to replace AFP. In the 2nd Edition of the International Classification of Headache Disorders (ICHD-2), PIFP is defined as "persistent facial pain that does not have the characteristics of the cranial neuralgias ... and is not attributed to another disorder." However, the term AFP continues to be used by the World Health Organization's 10th revision of the International Statistical Classification of Diseases and Related Health Problems and remains in general use by clinicians to refer to chronic facial pain that does not meet any diagnostic criteria and does not respond to most treatments.
Occipital nerve stimulation (ONS), also called peripheral nerve stimulation (PNS) of the occipital nerves, is used to treat chronic migraine patients who have failed to respond to pharmaceutical treatments.
Migraine treatment may be either prophylactic (preventive) or abortive (rescue). Prevention is better than cure, so the ideal treatment goal is to prevent migraine attacks. Because migraine is an exceedingly complex condition, there are various preventive treatments which have their effect by disrupting different links in the chain of events that occur during a migraine attack. As rescue treatments also target and disrupt different processes occurring during migraine, these are summarized, with their relative merits and demerits.

Occipital nerve block is a procedure involving injection of steroids or anesthetics into regions of the greater occipital nerve and the lesser occipital nerve used to treat chronic headaches.

Cervicocranial syndrome or is a neurological illness. It is a combination of symptoms that are caused by an abnormality in the neck. The bones of the neck that are affected are cervical vertebrae. This syndrome can be identified by confirming cervical bone shifts, collapsed cervical bones or misalignment of the cervical bone leading to improper functioning of cervical spinal nerves.Greenberg Regenerative Medicine | Bryn Mawr, Pennsylvania Cervicocranial syndrome is either congenital or acquired. Some examples of diseases that could result in cervicocranial syndrome are Chiari disease, Klippel-Feil malformation osteoarthritis, and trauma. Treatment options include neck braces, pain medication and surgery. The quality of life for individuals suffering from CCJ syndrome can improve through surgery.
References
- 1 2 3 4 5 6 7 Derek M, Kevin B (2020). "Occipital Neuralgia". Statpearls. PMID 30855865.
 Text was copied from this source, which is available under a Creative Commons Attribution 4.0 International License.
Text was copied from this source, which is available under a Creative Commons Attribution 4.0 International License. - ↑ Ansari, H.; Garza, I. (22 April 2012). "Occipital Neuralgia Secondary to a Spontaneous CSF Leak (P03.218)". Neurology. 78 (Meeting Abstracts 1): P03.218. doi:10.1212/WNL.78.1_MeetingAbstracts.P03.218.
- ↑ Gazelka, Halena M; Knievel, Sarah; Mauck, W. David; Moeschler, Susan; Pingree, Matthew; Rho, Richard; Lamer, Tim (April 2014). "Incidence of neuropathic pain after radiofrequency denervation of the third occipital nerve". Journal of Pain Research. 7: 195–8. doi: 10.2147/JPR.S60925 . PMC 3986282 . PMID 24748815.
- ↑ Moulding, HD; Bilsky, MH (March 2010). "Metastases to the craniovertebral junction". Neurosurgery. 66 (3 Suppl): 113–8. doi:10.1227/01.NEU.0000365829.97078.B2. PMID 20173512.
- ↑ De Santi, L; Annunziata, P (February 2012). "Clin Neurol Neurosurg". Clinical Neurology and Neurosurgery. 114 (2): 101–7. doi:10.1016/j.clineuro.2011.10.044. PMID 22130044. S2CID 3402581.