This article needs additional citations for verification .(April 2025) |
| Seminiferous tubule | |
|---|---|
 | |
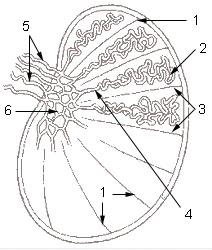 1: Testicular septa 2: Convoluted seminiferous tubules 3: Testicular lobules 4: Straight seminiferous tubules 5: Efferent ductules 6: Rete testis | |
| Details | |
| Identifiers | |
| Latin | tubuli seminiferi |
| MeSH | D012671 |
| TA98 | A09.3.01.022 |
| TA2 | 3599 |
| FMA | 19825 |
| Anatomical terminology | |
Seminiferous tubules are located within the testicles, and are the specific location of meiosis, and the subsequent creation of male gametes, namely spermatozoa.



