A testicle or testis is the male gonad in all bilaterians, including humans. It is homologous to the female ovary. The functions of the testicles are to produce both sperm and androgens, primarily testosterone. Testosterone release is controlled by the anterior pituitary luteinizing hormone, whereas sperm production is controlled both by the anterior pituitary follicle-stimulating hormone and gonadal testosterone.
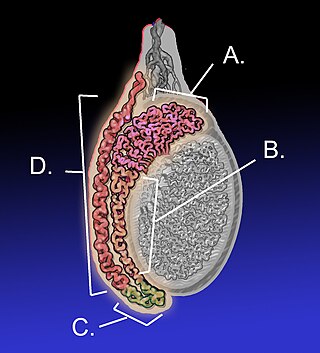
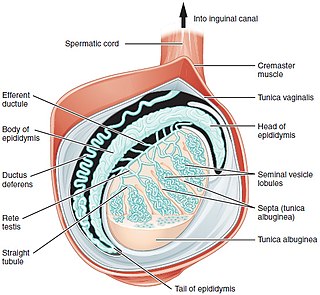
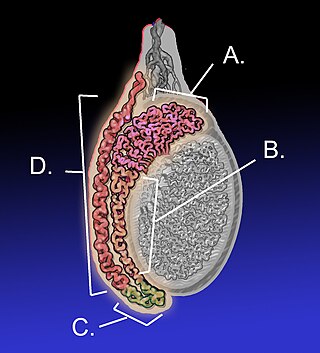
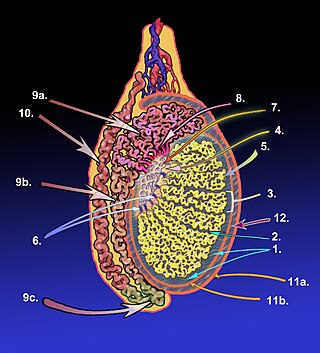
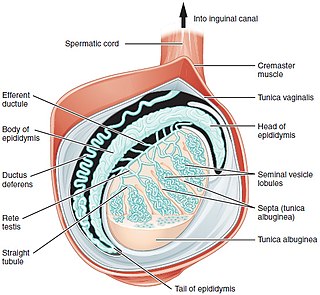
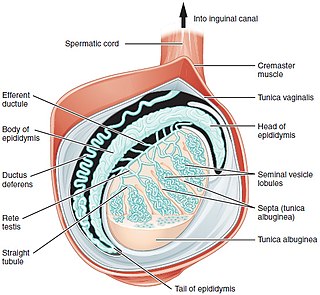
The epididymis is an elongated tubular structure attached to the posterior side of each one of the two male reproductive glands, the testicles. It is a single, narrow, tightly coiled tube in adult humans, 6 to 7 centimetres in length; uncoiled the tube would be approximately 6 m long. It connects the testicle to the vas deferens in the male reproductive system. The epididymis serves as an interconnection between the multiple efferent ducts at the rear of a testicle (proximally), and the vas deferens (distally). Its primary function is the storage, maturation and transport of sperm cells.

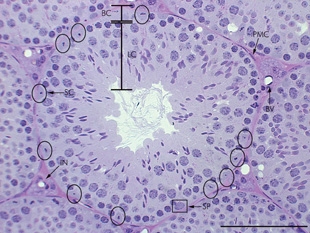
Leydig cells, also known as interstitial cells of the testes and interstitial cells of Leydig, are found adjacent to the seminiferous tubules in the testicle and produce testosterone in the presence of luteinizing hormone (LH). They are polyhedral in shape and have a large, prominent nucleus, an eosinophilic cytoplasm, and numerous lipid-filled vesicles.

Spermatogenesis is the process by which haploid spermatozoa develop from germ cells in the seminiferous tubules of the testicle. This process starts with the mitotic division of the stem cells located close to the basement membrane of the tubules. These cells are called spermatogonial stem cells. The mitotic division of these produces two types of cells. Type A cells replenish the stem cells, and type B cells differentiate into primary spermatocytes. The primary spermatocyte divides meiotically into two secondary spermatocytes; each secondary spermatocyte divides into two equal haploid spermatids by Meiosis II. The spermatids are transformed into spermatozoa (sperm) by the process of spermiogenesis. These develop into mature spermatozoa, also known as sperm cells. Thus, the primary spermatocyte gives rise to two cells, the secondary spermatocytes, and the two secondary spermatocytes by their subdivision produce four spermatozoa and four haploid cells.

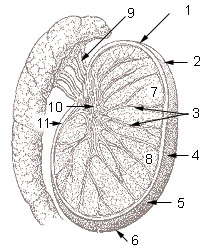
Seminiferous tubules are located within the testicles, and are the specific location of meiosis, and the subsequent creation of male gametes, namely spermatozoa.

The rete testis is an anastomosing network of delicate tubules located in the hilum of the testicle that carries sperm from the seminiferous tubules to the efferent ducts. It is the homologue of the rete ovarii in females. Its function is to provide a site for fluid reabsorption.
In biology, a tubule is a general term referring to small tube or similar type of structure. Specifically, tubule can refer to:

The mediastinum is the central compartment of the thoracic cavity. Surrounded by loose connective tissue, it is an undelineated region that contains a group of structures within the thorax, namely the heart and its vessels, the esophagus, the trachea, the phrenic and cardiac nerves, the thoracic duct, the thymus and the lymph nodes of the central chest.

The male reproductive system consists of a number of sex organs that play a role in the process of human reproduction. These organs are located on the outside of the body, and within the pelvis.

A seminoma is a germ cell tumor of the testicle or, more rarely, the mediastinum or other extra-gonadal locations. It is a malignant neoplasm and is one of the most treatable and curable cancers, with a survival rate above 95% if discovered in early stages.

The blood–testis barrier is a physical barrier between the blood vessels and the seminiferous tubules of the animal testes. The name "blood-testis barrier" is misleading as it is not a blood-organ barrier in a strict sense, but is formed between Sertoli cells of the seminiferous tubule and isolates the further developed stages of germ cells from the blood. A more correct term is the Sertoli cell barrier (SCB).
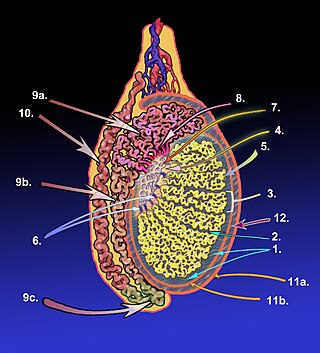
The tunica albugine is a dense, blue-white layer of fibrous tissue surrounding the testis. It is the middle of three enveloppes forming the capsule of the testis; it is deep to the visceral layer of tunica vaginalis, and superficial to the tunica vasculosa testis.
Testicular sperm extraction (TESE) is a surgical procedure in which a small portion of tissue is removed from the testicle and any viable sperm cells from that tissue are extracted for use in further procedures, most commonly intracytoplasmic sperm injection (ICSI) as part of in vitro fertilisation (IVF). TESE is often recommended to patients who cannot produce sperm by ejaculation due to azoospermia.
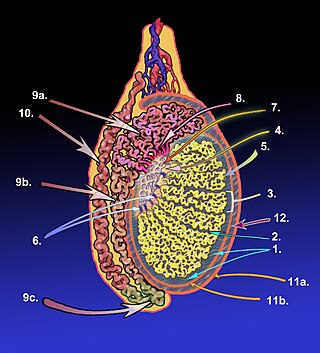
The mediastinum testis is a thick yet incomplete septum at the posterior part of the testis formed by the tunica albuginea of testis projecting into the testis at its posterior aspect where the testis is not lined by the serous membrane to allow for the attachment of the epididymis. It extends posteriorly between the testis' superior pole and inferior pole. It is wider superiorly than inferiorly. It supports the rete testis and blood and lymphatic vessels of the testis in their passage into and out of the substance of the gland.
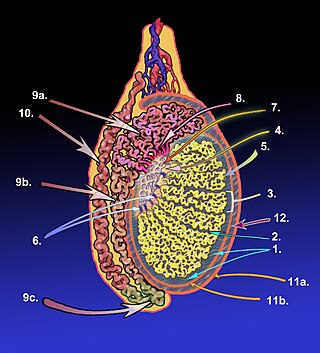
The septa testis are fibrous partitions of the testis dividing the testis into compartments - the lobules of the testis. The septa are formed by extensions of the tunica albuginea - the dense fibrous connective tissue surface covering of the testis - into the substance of the testis. The septa converge towards the mediastinum testis.
The development of the reproductive system is the part of embryonic growth that results in the sex organs and contributes to sexual differentiation. Due to its large overlap with development of the urinary system, the two systems are typically described together as the urogenital or genitourinary system.
The development of the gonads is part of the prenatal development of the reproductive system and ultimately forms the testicles in males and the ovaries in females. The gonads initially develop from the mesothelial layer of the peritoneum.

In most terrestrial mammals, the scrotum or scrotal sac is a part of the external male genitalia located at the base of the penis that consists of a suspended dual-chambered sac of skin and smooth muscle. The scrotum contains the external spermatic fascia, testicles, epididymides, and vasa deferentia. It is a distention of the perineum and carries some abdominal tissues into its cavity including the testicular artery, testicular vein, and pampiniform plexus. The perineal raphe is a small, vertical, slightly raised ridge of scrotal skin under which is found the scrotal septum. It appears as a thin longitudinal line that runs front to back over the entire scrotum. In humans, the scrotum becomes covered with pubic hair at puberty. The scrotum will usually tighten during penile erection and when exposed to cold temperatures. One testis is typically lower than the other to avoid compression in the event of an impact.

Scrotalultrasound is a medical ultrasound examination of the scrotum. It is used in the evaluation of testicular pain, and can help identify solid masses.
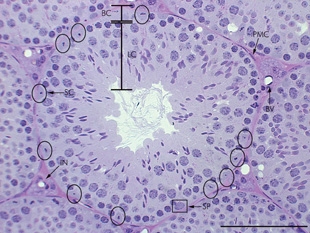
A peritubular myoid (PTM) cell is one of the smooth muscle cells which surround the seminiferous tubules in the testis. These cells are present in all mammals but their organization and abundance varies between species. The exact role of PTM cells is still somewhat uncertain and further work into this is needed. However, a number of functions of these cells have been established. They are contractile cells which contain actin filaments and are primarily involved in transport of spermatozoa through the tubules. They provide structural integrity to the tubules through their involvement in laying down the basement membrane. This has also been shown to affect Sertoli cell function and PTM cells also communicate with Sertoli cells through the secretion of growth factors and ECM components. Studies have shown PTM cells to be critical in achieving normal spermatogenesis. Overall, PTM cells have a role in both maintaining the structure of the tubules and regulating spermatogenesis through cellular interaction.