Urology, also known as genitourinary surgery, is the branch of medicine that focuses on surgical and medical diseases of the urinary-tract system and the reproductive organs. Organs under the domain of urology include the kidneys, adrenal glands, ureters, urinary bladder, urethra, and the male reproductive organs.
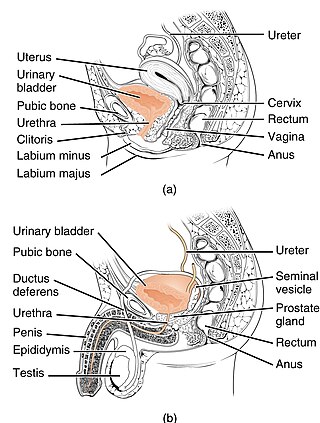
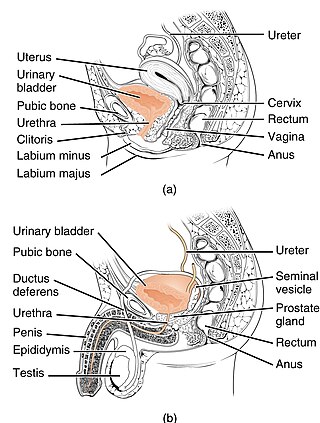
The urethra is a tube that connects the urinary bladder to the urinary meatus for the removal of urine from the body of both females and males. In human females and other primates, the urethra connects to the urinary meatus above the vagina, whereas in marsupials, the female's urethra empties into the urogenital sinus.

The prostate is both an accessory gland of the male reproductive system and a muscle-driven mechanical switch between urination and ejaculation. It is found only in some mammals. It differs between species anatomically, chemically, and physiologically. Anatomically, the prostate is found below the bladder, with the urethra passing through it. It is described in gross anatomy as consisting of lobes and in microanatomy by zone. It is surrounded by an elastic, fibromuscular capsule and contains glandular tissue as well as connective tissue.

The urinary system, also known as the urinary tract or renal system, consists of the kidneys, ureters, bladder, and the urethra. The purpose of the urinary system is to eliminate waste from the body, regulate blood volume and blood pressure, control levels of electrolytes and metabolites, and regulate blood pH. The urinary tract is the body's drainage system for the eventual removal of urine. The kidneys have an extensive blood supply via the renal arteries which leave the kidneys via the renal vein. Each kidney consists of functional units called nephrons. Following filtration of blood and further processing, wastes exit the kidney via the ureters, tubes made of smooth muscle fibres that propel urine towards the urinary bladder, where it is stored and subsequently expelled from the body by urination (voiding). The female and male urinary system are very similar, differing only in the length of the urethra.
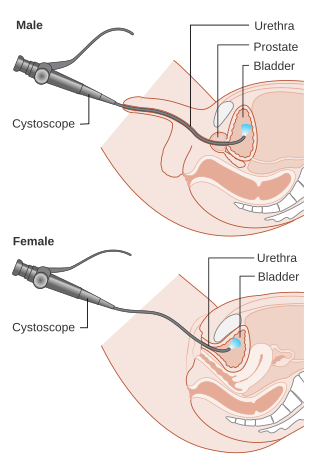
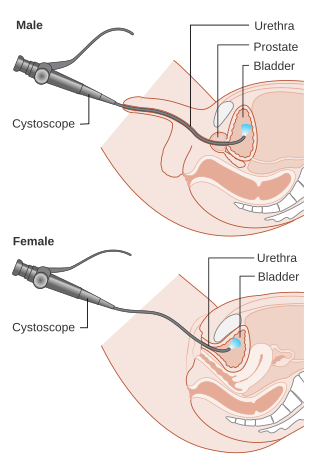
Cystoscopy is endoscopy of the urinary bladder via the urethra. It is carried out with a cystoscope.
The excretory system is a passive biological system that removes excess, unnecessary materials from the body fluids of an organism, so as to help maintain internal chemical homeostasis and prevent damage to the body. The dual function of excretory systems is the elimination of the waste products of metabolism and to drain the body of used up and broken down components in a liquid and gaseous state. In humans and other amniotes most of these substances leave the body as urine and to some degree exhalation, mammals also expel them through sweating.

Urination, also known as micturition, is the release of urine from the urinary bladder through the urethra to the outside of the body. It is the urinary system's form of excretion. It is also known medically as micturition, voiding, uresis, or, rarely, emiction, and known colloquially by various names including peeing, weeing, and pissing. In healthy humans, the process of urination is under voluntary control. In infants, some elderly individuals, and those with neurological injury, urination may occur as a reflex. It is normal for adult humans to urinate up to seven times during the day.

The ureters are tubes made of smooth muscle that propel urine from the kidneys to the urinary bladder. In a human adult, the ureters are usually 20–30 cm (8–12 in) long and around 3–4 mm (0.12–0.16 in) in diameter. The ureter is lined by urothelial cells, a type of transitional epithelium, and has an additional smooth muscle layer that assists with peristalsis in its lowest third.

The seminal vesicles are a pair of two convoluted tubular glands that lie behind the urinary bladder of some male mammals. They secrete fluid that partly composes the semen.

Hematuria or haematuria is defined as the presence of blood or red blood cells in the urine. "Gross hematuria" occurs when urine appears red, brown, or tea-colored due to the presence of blood. Hematuria may also be subtle and only detectable with a microscope or laboratory test. Blood that enters and mixes with the urine can come from any location within the urinary system, including the kidney, ureter, urinary bladder, urethra, and in men, the prostate. Common causes of hematuria include urinary tract infection (UTI), kidney stones, viral illness, trauma, bladder cancer, and exercise. These causes are grouped into glomerular and non-glomerular causes, depending on the involvement of the glomerulus of the kidney. But not all red urine is hematuria. Other substances such as certain medications and foods can cause urine to appear red. Menstruation in women may also cause the appearance of hematuria and may result in a positive urine dipstick test for hematuria. A urine dipstick test may also give an incorrect positive result for hematuria if there are other substances in the urine such as myoglobin, a protein excreted into urine during rhabdomyolysis. A positive urine dipstick test should be confirmed with microscopy, where hematuria is defined by three of more red blood cells per high power field. When hematuria is detected, a thorough history and physical examination with appropriate further evaluation can help determine the underlying cause.
Dysuria refers to painful or uncomfortable urination.

Urinary retention is an inability to completely empty the bladder. Onset can be sudden or gradual. When of sudden onset, symptoms include an inability to urinate and lower abdominal pain. When of gradual onset, symptoms may include loss of bladder control, mild lower abdominal pain, and a weak urine stream. Those with long-term problems are at risk of urinary tract infections.

Transitional epithelium also known as urothelium is a type of stratified epithelium. Transitional epithelium is a type of tissue that changes shape in response to stretching. The transitional epithelium usually appears cuboidal when relaxed and squamous when stretched. This tissue consists of multiple layers of epithelial cells which can contract and expand in order to adapt to the degree of distension needed. Transitional epithelium lines the organs of the urinary system and is known here as urothelium. The bladder for example has a need for great distension.

The detrusor muscle, also detrusor urinae muscle, muscularis propria of the urinary bladder and muscularis propria, is smooth muscle found in the wall of the bladder. The detrusor muscle remains relaxed to allow the bladder to store urine, and contracts during urination to release urine. Related are the urethral sphincter muscles which envelop the urethra to control the flow of urine when they contract.

The internal urethral sphincter is a urethral sphincter muscle which constricts the internal urethral orifice. It is located at the junction of the urethra with the urinary bladder and is continuous with the detrusor muscle, but anatomically and functionally fully independent from it. It is composed of smooth muscle, so it is under the control of the autonomic nervous system, specifically the sympathetic nervous system.
Urologic diseases or conditions include urinary tract infections, kidney stones, bladder control problems, and prostate problems, among others. Some urologic conditions do not affect a person for that long and some are lifetime conditions. Kidney diseases are normally investigated and treated by nephrologists, while the specialty of urology deals with problems in the other organs. Gynecologists may deal with problems of incontinence in women.
Feline idiopathic cystitis (FIC) or feline interstitial cystitis or cystitis in cats, is one of the most frequently observed forms of feline lower urinary tract disease (FLUTD). Feline cystitis means "inflammation of the bladder in cats". The term idiopathic means unknown cause; however, certain behaviours have been known to aggravate the illness once it has been initiated. It can affect both males and females of any breed of cat. It is more commonly found in female cats; however, when males do exhibit cystitis, it is usually more dangerous.

Urodynamic testing or urodynamics is a study that assesses how the bladder and urethra are performing their job of storing and releasing urine. Urodynamic tests can help explain symptoms such as:

Overflow incontinence is a concept of urinary incontinence, characterized by the involuntary release of urine from an overfull urinary bladder, often in the absence of any urge to urinate. This condition occurs in people who have a blockage of the bladder outlet, or when the muscle that expels urine from the bladder is too weak to empty the bladder normally. Overflow incontinence may also be a side effect of certain medications.

Ureteral cancer is cancer of the ureters, muscular tubes that propel urine from the kidneys to the urinary bladder. It is also known as ureter cancer, renal pelvic cancer, and rarely ureteric cancer or uretal cancer. Cancer in this location is rare. Ureteral cancer becomes more likely in older adults, usually ages 70–80, who have previously been diagnosed with bladder cancer.