The seminal vesicles are a pair of convoluted tubular accessory glands that lie behind the urinary bladder of male mammals. They secrete fluid that partly composes the semen.

The vas deferens, with the more modern name ductus deferens, is part of the male reproductive system of many vertebrates. The ducts transport sperm from the epididymides to the ejaculatory ducts in anticipation of ejaculation. The vas deferens is a partially coiled tube which exits the abdominal cavity through the inguinal canal.

The ejaculatory ducts are paired structures in the male reproductive system. Each ejaculatory duct is formed by the union of the vas deferens with the duct of the seminal vesicle. They pass through the prostate, and open into the urethra above the seminal colliculus. During ejaculation, semen passes through the prostate gland, enters the urethra and exits the body via the urinary meatus.

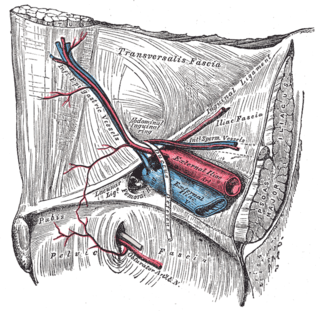
The spermatic cord is the cord-like structure in males formed by the vas deferens and surrounding tissue that runs from the deep inguinal ring down to each testicle. Its serosal covering, the tunica vaginalis, is an extension of the peritoneum that passes through the transversalis fascia. Each testicle develops in the lower thoracic and upper lumbar region and migrates into the scrotum. During its descent it carries along with it the vas deferens, its vessels, nerves etc. There is one on each side.

The inguinal canal is a passage in the anterior abdominal wall on each side of the body, which in males, convey the spermatic cords and in females, the round ligament of the uterus. The inguinal canals are larger and more prominent in males.

The external iliac veins are large veins that connect the femoral veins to the common iliac veins. Their origin is at the inferior margin of the inguinal ligaments and they terminate when they join the internal iliac veins.
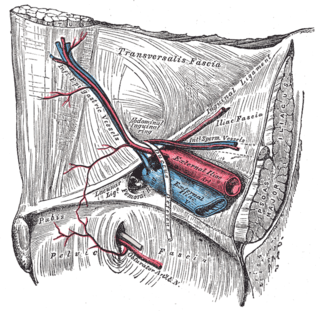
In human anatomy, the inferior epigastric artery is an artery that arises from the external iliac artery. It is accompanied by the inferior epigastric vein; inferiorly, these two inferior epigastric vessels together travel within the lateral umbilical fold The inferior epigastric artery then traverses the arcuate line of rectus sheath to enter the rectus sheath, then anastomoses with the superior epigastric artery within the rectus sheath.

The lumbar plexus is a web of nerves in the lumbar region of the body which forms part of the larger lumbosacral plexus. It is formed by the divisions of the first four lumbar nerves (L1-L4) and from contributions of the subcostal nerve (T12), which is the last thoracic nerve. Additionally, the ventral rami of the fourth lumbar nerve pass communicating branches, the lumbosacral trunk, to the sacral plexus. The nerves of the lumbar plexus pass in front of the hip joint and mainly support the anterior part of the thigh.
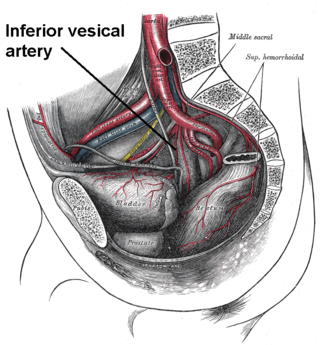
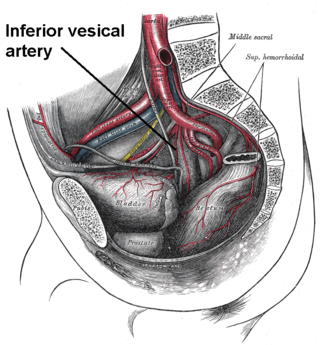
The inferior vesical artery is an artery of the pelvis which arises from the internal iliac artery and supplies parts of the urinary bladder as well as other structures of the urinary system and structures of the male reproductive system.

The superior vesical artery supplies numerous branches to the upper part of the bladder. This artery often also gives branches to the vas deferens and can provide minor collateral circulation for the testicles.

The abdominal aortic plexus is formed by branches derived, on either side, from the celiac plexus and ganglia, and receives filaments from some of the lumbar ganglia.

The spermatic plexus is derived from the renal plexus, receiving branches from the aortic plexus. It accompanies the internal spermatic artery to the testis.

The testicular artery is a branch of the abdominal aorta that supplies blood to the testicle. It is a paired artery, with one for each of the testicles.

The testicular vein, the male gonadal vein, carries deoxygenated blood from its corresponding testis to the inferior vena cava or one of its tributaries. It is the male equivalent of the ovarian vein, and is the venous counterpart of the testicular artery.

The cremasteric artery is a branch of the inferior epigastric artery which accompanies the spermatic cord to supply the cremaster muscle as well as other coverings of the spermatic cord in the male.

The inferior hypogastric plexus is a network of nerves that supplies the organs of the pelvic cavity. The inferior hypogastric plexus gives rise to the prostatic plexus in males and the uterovaginal plexus in females.

The artery to the ductus deferens is an artery in males that provides blood to the ductus deferens.

The muscular layer is a region of muscle in many organs in the vertebrate body, adjacent to the submucosa. It is responsible for gut movement such as peristalsis. The Latin, tunica muscularis, may also be used.

The pampiniform plexus is a venous plexus – a network of many small veins found in the human male spermatic cord, and the suspensory ligament of the ovary. In the male, it is formed by the union of multiple testicular veins from the back of the testis and tributaries from the epididymis.
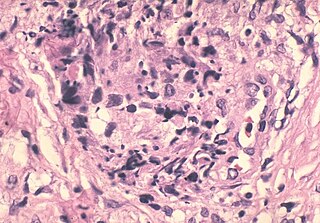
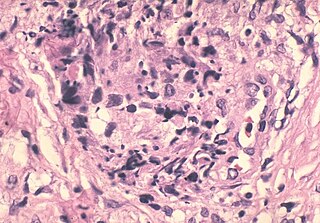
A sperm granuloma is a lump of leaked sperm that appears along the vasa deferentia or epididymides in vasectomized individuals. While the majority of sperm granulomas are present along the vas deferens, the rest of them form at the epididymis. Sperm granulomas range in size, from one millimeter to one centimeter. They consist of a central mass of degenerating sperm surrounded by tissue containing blood vessels and immune system cells. Sperm granulomas may also have a yellow, white, or cream colored center when cut open. While some sperm granulomas can be painful, most of them are painless and asymptomatic. Sperm granulomas can appear as a result of surgery, trauma, or an infection. They can appear as early as four days after surgery and fully formed ones can appear as late as 208 days later.