This article needs additional citations for verification .(December 2018) |
| Anal canal | |
|---|---|
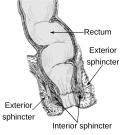
 Anatomy of the anus and rectum | |
 Coronal section through the anal canal. B. Cavity of urinary bladder V.D. Ductus deferens. S.V. Seminal vesicle. R. Second part of rectum. A.C. Anal canal. L.A. Levator ani. I.S. Sphincter ani internus. E.S. Sphincter ani externus. | |
| Details | |
| Precursor | Hindgut, proctodeum |
| Artery | Superior rectal artery (above pectinate line) and inferior rectal artery (below line) |
| Vein | Superior rectal vein (above pectinate line) and Inferior rectal vein (below line) |
| Nerve | Autonomic inferior hypogastric plexus (above pectinate line) and somatic inferior rectal nerves (below line) |
| Lymph | Superficial inguinal lymph node (below pectinate line) and internal iliac lymph nodes (above line) |
| Identifiers | |
| Latin | canalis analis |
| MeSH | D001003 |
| TA98 | A05.7.05.001 |
| TA2 | 3009 |
| FMA | 15703 |
| Anatomical terminology | |
The anal canal is the part that connects the rectum to the anus, located below the level of the pelvic diaphragm. [1] It is located within the anal triangle of the perineum, between the right and left ischioanal fossae. As the final functional segment of the bowel, it functions to regulate release of feces by two muscular anal sphincter complexes. The anus is the aperture at the terminal portion of the anal canal.