Related Research Articles

The ileum is the final section of the small intestine in most higher vertebrates, including mammals, reptiles, and birds. In fish, the divisions of the small intestine are not as clear and the terms posterior intestine or distal intestine may be used instead of ileum. Its main function is to absorb vitamin B12, bile salts, and whatever products of digestion that were not absorbed by the jejunum.

The jejunum is the second part of the small intestine in humans and most higher vertebrates, including mammals, reptiles, and birds. Its lining is specialized for the absorption by enterocytes of small nutrient molecules which have been previously digested by enzymes in the duodenum.

Immunoglobulin A is an antibody that plays a role in the immune function of mucous membranes. The amount of IgA produced in association with mucosal membranes is greater than all other types of antibody combined. In absolute terms, between three and five grams are secreted into the intestinal lumen each day. This represents up to 15% of total immunoglobulins produced throughout the body.

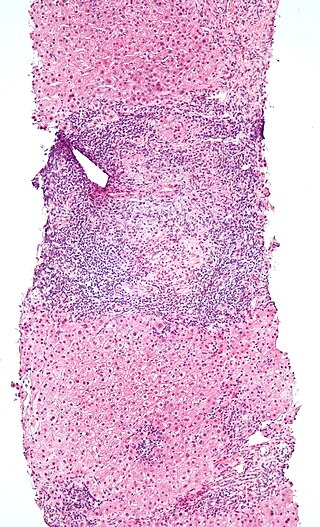
Peyer's patches are organized lymphoid follicles, named after the 17th-century Swiss anatomist Johann Conrad Peyer. They are an important part of gut associated lymphoid tissue usually found in humans in the lowest portion of the small intestine, mainly in the distal jejunum and the ileum, but also could be detected in the duodenum.
Gut-associated lymphoid tissue (GALT) is a component of the mucosa-associated lymphoid tissue (MALT) which works in the immune system to protect the body from invasion in the gut.
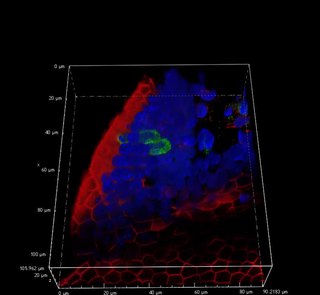
The mucosa-associated lymphoid tissue (MALT), also called mucosa-associated lymphatic tissue, is a diffuse system of small concentrations of lymphoid tissue found in various submucosal membrane sites of the body, such as the gastrointestinal tract, nasopharynx, thyroid, breast, lung, salivary glands, eye, and skin. MALT is populated by lymphocytes such as T cells and B cells, as well as plasma cells, dendritic cells and macrophages, each of which is well situated to encounter antigens passing through the mucosal epithelium. The appendix, long misunderstood as a vestigial organ, is now recognized as a key MALT structure, playing an essential role in B-lymphocyte-mediated immune responses, hosting extrathymically derived T-lymphocytes, regulating pathogens through its lymphatic vessels, and potentially producing early defenses against diseases. In the case of intestinal MALT, M cells are also present, which sample antigen from the lumen and deliver it to the lymphoid tissue. MALT constitute about 50% of the lymphoid tissue in human body. Immune responses that occur at mucous membranes are studied by mucosal immunology.
Intestinal permeability is a term describing the control of material passing from inside the gastrointestinal tract through the cells lining the gut wall, into the rest of the body. The intestine normally exhibits some permeability, which allows nutrients to pass through the gut, while also maintaining a barrier function to keep potentially harmful substances from leaving the intestine and migrating to the body more widely. In a healthy human intestine, small particles can migrate through tight junction claudin pore pathways, and particles up to 10–15 Å can transit through the paracellular space uptake route. There is some evidence abnormally increased intestinal permeability may play a role in some chronic diseases and inflammatory conditions. The most well understood condition with observed increased intestinal permeability is celiac disease.
Immune tolerance, also known as immunological tolerance or immunotolerance, refers to the immune system's state of unresponsiveness to substances or tissues that would otherwise trigger an immune response. It arises from prior exposure to a specific antigen and contrasts the immune system's conventional role in eliminating foreign antigens. Depending on the site of induction, tolerance is categorized as either central tolerance, occurring in the thymus and bone marrow, or peripheral tolerance, taking place in other tissues and lymph nodes. Although the mechanisms establishing central and peripheral tolerance differ, their outcomes are analogous, ensuring immune system modulation.
Lymphotoxin is a member of the tumor necrosis factor (TNF) superfamily of cytokines, whose members are responsible for regulating the growth and function of lymphocytes and are expressed by a wide variety of cells in the body.
Intraepithelial lymphocytes (IEL) are lymphocytes found in the epithelial layer of mammalian mucosal linings, such as the gastrointestinal (GI) tract and reproductive tract. However, unlike other T cells, IELs do not need priming. Upon encountering antigens, they immediately release cytokines and cause killing of infected target cells. In the GI tract, they are components of gut-associated lymphoid tissue (GALT).
Lymphocyte homing receptors are cell adhesion molecules expressed on lymphocyte cell membranes that recognize addressins on target tissues. Lymphocyte homing refers to adhesion of the circulating lymphocytes in blood to specialized endothelial cells within lymphoid organs. These diverse tissue-specific adhesion molecules on lymphocytes and on endothelial cells contribute to the development of specialized immune responses.

Lymphotoxin-alpha (LT-α) formerly known as tumor necrosis factor-beta (TNF-β) is a protein that in humans is encoded by the LTA gene. Belonging to the hematopoietic cell line, LT-α exhibits anti-proliferative activity and causes the cellular destruction of tumor cell lines. As a cytotoxic protein, LT-α performs a variety of important roles in immune regulation depending on the form that it is secreted as. Unlike other members of the TNF superfamily, LT-α is only found as a soluble homotrimer, when found at the cell surface it is found only as a heterotrimer with LTβ.

The intestinal epithelium is the single cell layer that forms the luminal surface (lining) of both the small and large intestine (colon) of the gastrointestinal tract. Composed of simple columnar epithelium its main functions are absorption, and secretion. Useful substances are absorbed into the body, and the entry of harmful substances is restricted. Secretions include mucins, and peptides.

Long-term close-knit interactions between symbiotic microbes and their host can alter host immune system responses to other microorganisms, including pathogens, and are required to maintain proper homeostasis. The immune system is a host defense system consisting of anatomical physical barriers as well as physiological and cellular responses, which protect the host against harmful microorganisms while limiting host responses to harmless symbionts. Humans are home to 1013 to 1014 bacteria, roughly equivalent to the number of human cells, and while these bacteria can be pathogenic to their host most of them are mutually beneficial to both the host and bacteria.

Mucosal immunology is the study of immune system responses that occur at mucosal membranes of the intestines, the urogenital tract, and the respiratory system. The mucous membranes are in constant contact with microorganisms, food, and inhaled antigens. In healthy states, the mucosal immune system protects the organism against infectious pathogens and maintains a tolerance towards non-harmful commensal microbes and benign environmental substances. Disruption of this balance between tolerance and deprivation of pathogens can lead to pathological conditions such as food allergies, irritable bowel syndrome, susceptibility to infections, and more.
Gut-specific homing is the mechanism by which activated T cells and antibody-secreting cells (ASCs) are targeted to both inflamed and non-inflamed regions of the gut in order to provide an effective immune response. This process relies on the key interaction between the integrin α4β7 and the addressin MadCAM-1 on the surfaces of the appropriate cells. Additionally, this interaction is strengthened by the presence of CCR9, a chemokine receptor, which interacts with TECK. Vitamin A-derived retinoic acid regulates the expression of these cell surface proteins.
Tuft cells are chemosensory cells in the epithelial lining of the intestines. Similar tufted cells are found in the respiratory epithelium where they are known as brush cells. The name "tuft" refers to the brush-like microvilli projecting from the cells. Ordinarily there are very few tuft cells present but they have been shown to greatly increase at times of a parasitic infection. Several studies have proposed a role for tuft cells in defense against parasitic infection. In the intestine, tuft cells are the sole source of secreted interleukin 25 (IL-25).

The intestinal mucosal barrier, also referred to as intestinal barrier, refers to the property of the intestinal mucosa that ensures adequate containment of undesirable luminal contents within the intestine while preserving the ability to absorb nutrients. The separation it provides between the body and the gut prevents the uncontrolled translocation of luminal contents into the body proper. Its role in protecting the mucosal tissues and circulatory system from exposure to pro-inflammatory molecules, such as microorganisms, toxins, and antigens is vital for the maintenance of health and well-being. Intestinal mucosal barrier dysfunction has been implicated in numerous health conditions such as: food allergies, microbial infections, irritable bowel syndrome, inflammatory bowel disease, celiac disease, metabolic syndrome, non-alcoholic fatty liver disease, diabetes, and septic shock.
Nasal- or nasopharynx- associated lymphoid tissue (NALT) represents immune system of nasal mucosa and is a part of mucosa-associated lymphoid tissue (MALT) in mammals. It protects body from airborne viruses and other infectious agents. In humans, NALT is considered analogous to Waldeyer's ring.

Type 3 innate lymphoid cells (ILC3) are immune cells from the lymphoid lineage that are part of the innate immune system. These cells participate in innate mechanisms on mucous membranes, contributing to tissue homeostasis, host-commensal mutualism and pathogen clearance. They are part of a heterogeneous group of innate lymphoid cells, which is traditionally divided into three subsets based on their expression of master transcription factors as well as secreted effector cytokines - ILC1, ILC2 and ILC3.
References
- 1 2 Mabbott NA, Donaldson DS, Ohno H, Williams IR, Mahajan A (July 2013). "Microfold (M) cells: important immunosurveillance posts in the intestinal epithelium". Mucosal Immunology. 6 (4): 666–677. doi:10.1038/mi.2013.30. PMC 3686595 . PMID 23695511.
- ↑ Miller H, Zhang J, Kuolee R, Patel GB, Chen W (March 2007). "Intestinal M cells: the fallible sentinels?". World Journal of Gastroenterology. 13 (10): 1477–1486. doi: 10.3748/wjg.v13.i10.1477 . PMC 1876659 . PMID 17461437.
- 1 2 Kanaya T, Ohno H (2014). "The Mechanisms of M-cell Differentiation". Bioscience of Microbiota, Food and Health. 33 (3): 91–97. doi:10.12938/bmfh.33.91. PMC 4098651 . PMID 25032083.
- ↑ Kraehenbuhl JP, Neutra MR (2000). "Epithelial M cells: differentiation and function". Annual Review of Cell and Developmental Biology. 16: 301–332. doi:10.1146/annurev.cellbio.16.1.301. PMID 11031239. Link
- ↑ Knoop KA, Kumar N, Butler BR, Sakthivel SK, Taylor RT, Nochi T, et al. (November 2009). "RANKL is necessary and sufficient to initiate development of antigen-sampling M cells in the intestinal epithelium". Journal of Immunology. 183 (9): 5738–5747. doi:10.4049/jimmunol.0901563. PMC 2922944 . PMID 19828638.
- ↑ Tahoun A, Mahajan S, Paxton E, Malterer G, Donaldson DS, Wang D, et al. (November 2012). "Salmonella transforms follicle-associated epithelial cells into M cells to promote intestinal invasion". Cell Host & Microbe. 12 (5): 645–656. doi: 10.1016/j.chom.2012.10.009 . PMID 23159054.
- ↑ Ohno H, Kanaya T, Williams IR (November 2012). "M cell differentiation: distinct lineage or phenotypic transition? Salmonella provides answers". Cell Host & Microbe. 12 (5): 607–609. doi: 10.1016/j.chom.2012.11.003 . PMID 23159049.
- ↑ Tahoun A, Mahajan S, Paxton E, Malterer G, Donaldson DS, Wang D, et al. (November 2012). "Salmonella transforms follicle-associated epithelial cells into M cells to promote intestinal invasion". Cell Host & Microbe. 12 (5): 645–656. doi: 10.1016/j.chom.2012.10.009 . PMID 23159054.
- ↑ Murphy KM (2012). Janeway's Immunobiology (8th ed.). New York: Garland Science. ISBN 978-0-8153-4243-4.
- ↑ Milligan L (April 2013). "From Mother's Gut to Milk". International Milk Genomics Consortium. Retrieved 2019-02-20.
- ↑ Ouzilou L, Caliot E, Pelletier I, Prévost MC, Pringault E, Colbère-Garapin F (September 2002). "Poliovirus transcytosis through M-like cells". The Journal of General Virology. 83 (Pt 9): 2177–2182. doi: 10.1099/0022-1317-83-9-2177 . PMID 12185271.
- ↑ Fotopoulos G, Harari A, Michetti P, Trono D, Pantaleo G, Kraehenbuhl JP (July 2002). "Transepithelial transport of HIV-1 by M cells is receptor-mediated". Proceedings of the National Academy of Sciences of the United States of America. 99 (14): 9410–9414. Bibcode:2002PNAS...99.9410F. doi: 10.1073/pnas.142586899 . PMC 123154 . PMID 12093918.