This article may require cleanup to meet Wikipedia's quality standards. The specific problem is: Content under Pubococcygeus and Puborectalis sections should be integrated with the rest of the article.(July 2020) |
| Levator ani | |
|---|---|
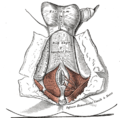
 Left levator ani seen from within. | |
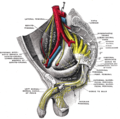
 Coronal section through the male anal canal. B. Cavity of urinary bladder V.D. Vas deferens. S.V. Seminal vesicle. R. Second part of rectum. A.C. Anal canal. L.A. Levator ani. I.S. Internal anal sphincter. E.S External anal sphincter. | |
| Details | |
| Origin | Inner surface of the side of the lesser pelvis |
| Insertion | Inner surface of coccyx, levator ani of opposite side, and into structures that penetrate it. |
| Artery | Inferior gluteal artery |
| Nerve | Pubococcygeus and iliococcygeus : |
| Actions | Supports the viscera in pelvic cavity |
| Identifiers | |
| Latin | musculus levator ani |
| TA98 | A04.5.04.002 |
| TA2 | 2403 |
| FMA | 19087 |
| Anatomical terms of muscle | |

The levator ani is a broad, thin muscle group, situated on either side of the pelvis. It is formed from three muscle components: the puborectalis, pubococcygeus, and the iliococcygeus. [3]
Contents
- Structure
- Origin and insertion
- Innervation
- Variation
- Pubococcygeus muscle
- Structure 2
- Function
- Kegel exercises
- Puborectalis muscle
- Function 2
- Clinical significance
- Levator ani syndrome
- Additional images
- See also
- References
- External links
It is attached to the inner surface of each side of the lesser pelvis, and these unite to form the greater part of the pelvic floor. The coccygeus muscle completes the pelvic floor, which is also called the pelvic diaphragm.
It supports the viscera in the pelvic cavity, and surrounds the various structures that pass through it.
The levator ani is the main pelvic floor muscle and contracts rhythmically during female orgasm, and painfully during vaginismus. [4]