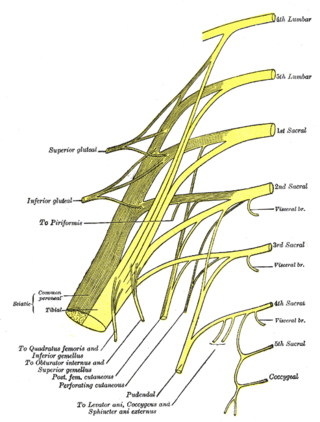
The pudendal nerve is the main nerve of the perineum. It is a mixed nerve and also conveys sympathetic autonomic fibers. It carries sensation from the external genitalia of both sexes and the skin around the anus and perineum, as well as the motor supply to various pelvic muscles, including the male or female external urethral sphincter and the external anal sphincter.

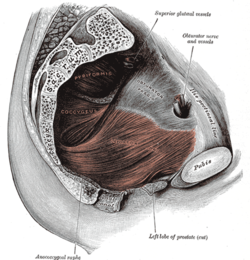
The levator ani is a broad, thin muscle group, situated on either side of the pelvis. It is formed from three muscle components: the pubococcygeus, the iliococcygeus, and the puborectalis.

The coccyx, commonly referred to as the tailbone, is the final segment of the vertebral column in all apes, and analogous structures in certain other mammals such as horses. In tailless primates since Nacholapithecus, the coccyx is the remnant of a vestigial tail. In animals with bony tails, it is known as tailhead or dock, in bird anatomy as tailfan. It comprises three to five separate or fused coccygeal vertebrae below the sacrum, attached to the sacrum by a fibrocartilaginous joint, the sacrococcygeal symphysis, which permits limited movement between the sacrum and the coccyx.
Pudendal nerve entrapment (PNE), also known as Alcock canal syndrome, is an uncommon source of chronic pain in which the pudendal nerve is entrapped or compressed in Alcock's canal. There are several different types of PNE based on the site of entrapment anatomically. Pain is positional and is worsened by sitting. Other symptoms include genital numbness, fecal incontinence and urinary incontinence.
Coccydynia is a medical term meaning pain in the coccyx or tailbone area, often brought on by a fall onto the coccyx or by persistent irritation usually from sitting.

The internal pudendal artery is one of the three pudendal arteries. It branches off the internal iliac artery, and provides blood to the external genitalia.

The piriformis muscle is a flat, pyramidally-shaped muscle in the gluteal region of the lower limbs. It is one of the six muscles in the lateral rotator group.

The internal obturator muscle or obturator internus muscle originates on the medial surface of the obturator membrane, the ischium near the membrane, and the rim of the pubis.
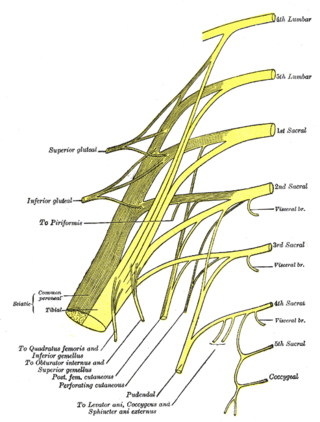
The anococcygeal nerve is a sensory nerve of the pelvis that arises from the coccygeal plexus. It pierces the coccygeus muscle and the sacrotuberous ligament to supply a small area of skin between the coccyx and anus, as well as the sacrococcygeal joint. The number of anococcygeal nerves varies between one and three.
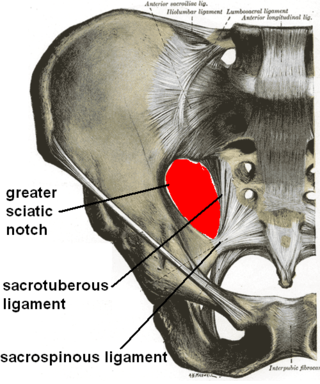
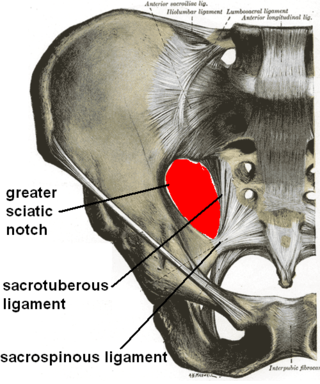
The sacrotuberous ligament is situated at the lower and back part of the pelvis. It is flat, and triangular in form; narrower in the middle than at the ends.
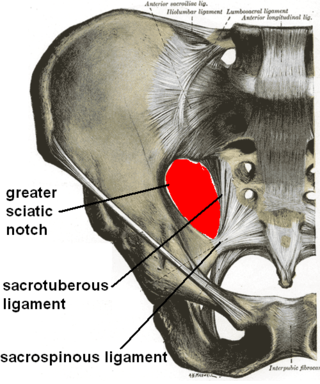
The sacrospinous ligament is a thin, triangular ligament in the human pelvis. The base of the ligament is attached to the outer edge of the sacrum and coccyx, and the tip of the ligament attaches to the spine of the ischium, a bony protuberance on the human pelvis. Its fibres are intermingled with the sacrotuberous ligament.

The lateral sacral arteries is an artery in the pelvis that arises from the posterior division of the internal iliac artery. It later splits into two smaller branches, a superior and an inferior.

The inferior gluteal artery is a terminal branch of the anterior trunk of the internal iliac artery. It exits the pelvis through the greater sciatic foramen. It is distributed chiefly to the buttock and the back of the thigh.

The perineal nerve is a nerve of the pelvis. It arises from the pudendal nerve in the pudendal canal. It gives superficial branches to the skin, and a deep branch to muscles. It supplies the skin and muscles of the perineum. Its latency is tested with electrodes.
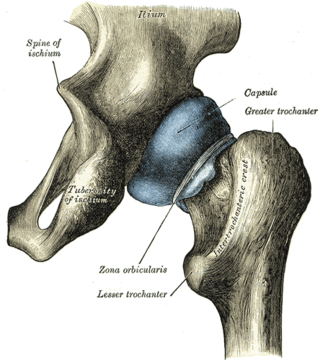
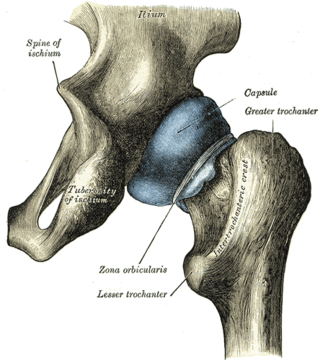
The ischial spine is part of the posterior border of the body of the ischium bone of the pelvis. It is a thin and pointed triangular eminence, more or less elongated in different subjects.

The anococcygeal body is a fibrous median raphe in the floor of the pelvis, which extends between the coccyx and the margin of the anus. It is composed of fibers of the levator ani muscle that unite with the muscle of the opposite side, muscle fibres from external anal sphincter, and fibrous connective tissue.
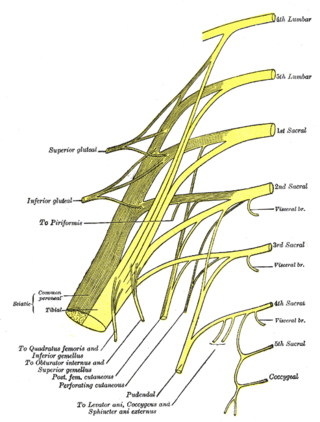
The nerve to obturator internus is a mixed nerve providing motor innervation to the obturator internus muscle and gemellus superior muscle, and sensory innervation to the hip joint. It is a branch of the sacral plexus. It is one of the group of deep gluteal nerves.
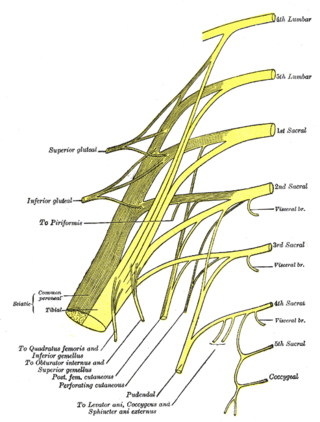
The coccygeal plexus is a small nervous plexus upon the pelvic (anterior) surface of the coccygeus muscle.

The anal triangle is the posterior part of the perineum. It contains the anal canal.

The vaginal support structures are those muscles, bones, ligaments, tendons, membranes and fascia, of the pelvic floor that maintain the position of the vagina within the pelvic cavity and allow the normal functioning of the vagina and other reproductive structures in the female. Defects or injuries to these support structures in the pelvic floor leads to pelvic organ prolapse. Anatomical and congenital variations of vaginal support structures can predispose a woman to further dysfunction and prolapse later in life. The urethra is part of the anterior wall of the vagina and damage to the support structures there can lead to incontinence and urinary retention.