| Anal triangle | |
|---|---|
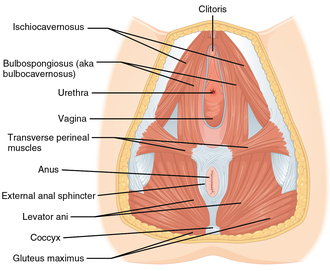 Muscles of the female perineum. (Anal triangle is roughly equal to bottom half of diagram.) | |
 Muscles of the male perineum. (Anal triangle is roughly equal to bottom half of diagram.) | |
| Details | |
| Identifiers | |
| Latin | regio analis |
| TA98 | A01.2.06.002 |
| TA2 | 278 |
| FMA | 20347 |
| Anatomical terminology | |
The anal triangle is the posterior part of the perineum. It contains the anus in mammals.