Related Research Articles
An artificial organ is a human made organ device or tissue that is implanted or integrated into a human — interfacing with living tissue — to replace a natural organ, to duplicate or augment a specific function or functions so the patient may return to a normal life as soon as possible. The replaced function does not have to be related to life support, but it often is. For example, replacement bones and joints, such as those found in hip replacements, could also be considered artificial organs.
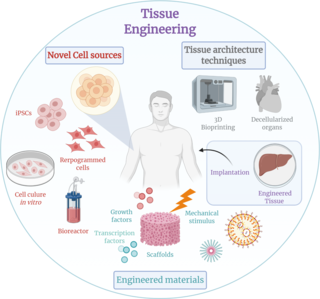
Tissue engineering is a biomedical engineering discipline that uses a combination of cells, engineering, materials methods, and suitable biochemical and physicochemical factors to restore, maintain, improve, or replace different types of biological tissues. Tissue engineering often involves the use of cells placed on tissue scaffolds in the formation of new viable tissue for a medical purpose but is not limited to applications involving cells and tissue scaffolds. While it was once categorized as a sub-field of biomaterials, having grown in scope and importance it can be considered as a field of its own.

A urethral stricture is a narrowing of the urethra, the tube connected to the bladder that allows the passing of urine. The narrowing reduces the flow of urine and makes it more difficult or even painful to empty the bladder.
Organ culture is the cultivation of either whole organs or parts of organs in vitro. It is a development from tissue culture methods of research, as the use of the actual in vitro organ itself allows for more accurate modelling of the functions of an organ in various states and conditions.
Allotransplant is the transplantation of cells, tissues, or organs to a recipient from a genetically non-identical donor of the same species. The transplant is called an allograft, allogeneic transplant, or homograft. Most human tissue and organ transplants are allografts.
In anatomy, a stoma is any opening in the body. For example, a mouth, a nose, and an anus are natural stomata. Any hollow organ can be manipulated into an artificial stoma as necessary. This includes the esophagus, stomach, duodenum, ileum, colon, pleural cavity, ureters, urinary bladder, and renal pelvis. Such a stoma may be permanent or temporary.
Müllerian agenesis, also known as Müllerian aplasia, vaginal agenesis, or Mayer-Rokitansky-Küster-Hauser syndrome, is a congenital malformation characterized by a failure of the Müllerian ducts to develop, resulting in a missing uterus and variable degrees of vaginal hypoplasia of its upper portion. Müllerian agenesis is the cause in 15% of cases of primary amenorrhoea. Because most of the vagina does not develop from the Müllerian duct, instead developing from the urogenital sinus, along with the bladder and urethra, it is present even when the Müllerian duct is completely absent. Because ovaries do not develop from the Müllerian ducts, affected people might have normal secondary sexual characteristics but are infertile due to the lack of a functional uterus. However, parenthood is possible through use of gestational surrogates.
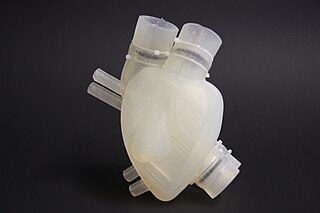
Organ printing utilizes techniques similar to conventional 3D printing where a computer model is fed into a printer that lays down successive layers of plastics or wax until a 3D object is produced. In the case of organ printing, the material being used by the printer is a biocompatible plastic. The biocompatible plastic forms a scaffold that acts as the skeleton for the organ that is being printed. As the plastic is being laid down, it is also seeded with human cells from the patient's organ that is being printed for. After printing, the organ is transferred to an incubation chamber to give the cells time to grow. After a sufficient amount of time, the organ is implanted into the patient.
Autotransplantation is the transplantation of organs, tissues, or even particular proteins from one part of the body to another in the same person.

Stress incontinence, also known as stress urinary incontinence (SUI) or effort incontinence is a form of urinary incontinence. It is due to inadequate closure of the bladder outlet by the urethral sphincter.

Veterinary surgery is surgery performed on animals by veterinarians, whereby the procedures fall into three broad categories: orthopaedics, soft tissue surgery, and neurosurgery. Advanced surgical procedures such as joint replacement, fracture repair, stabilization of cranial cruciate ligament deficiency, oncologic (cancer) surgery, herniated disc treatment, complicated gastrointestinal or urogenital procedures, kidney transplant, skin grafts, complicated wound management, and minimally invasive procedures are performed by veterinary surgeons. Most general practice veterinarians perform routine surgeries such as neuters and minor mass excisions; some also perform additional procedures.
Penis transplantation is a surgical transplant procedure in which a penis is transplanted to a patient. The penis may be an allograft from a human donor, or it may be grown artificially, though the latter has not yet been transplanted onto a human.

Anthony Atala, M.D., is an American bioengineer, urologist, and pediatric surgeon. He is the W.H. Boyce professor of urology, the founding director of the Wake Forest Institute for Regenerative Medicine, and the chair of the Department of Urology at Wake Forest School of Medicine in North Carolina. His work focuses on the science of regenerative medicine: "a practice that aims to refurbish diseased or damaged tissue using the body's own healthy cells".
The Wake Forest Institute for Regenerative Medicine (WFIRM) is a research institute affiliated with Wake Forest School of Medicine and located in Winston-Salem, North Carolina, United States
Transplantable organs and tissues may refer to both organs and tissues that are relatively often transplanted, as well as organs and tissues which are relatively seldom transplanted. In addition to this it may also refer to possible-transplants which are still in the experimental stage.
In tissue engineering, neo-organ is the final structure of a procedure based on transplantation consisting of endogenous stem/progenitor cells grown ex vivo within predesigned matrix scaffolds. Current organ donation faces the problems of patients waiting to match for an organ and the possible risk of the patient's body rejecting the organ. Neo-organs are being researched as a solution to those problems with organ donation. Suitable methods for creating neo-organs are still under development. One experimental method is using adult stem cells, which use the patients own stem cells for organ donation. Currently this method can be combined with decellularization, which uses a donor organ for structural support but removes the donors cells from the organ. Similarly, the concept of 3-D bioprinting organs has shown experimental success in printing bioink layers that mimic the layer of organ tissues. However, these bioinks do not provide structural support like a donor organ. Current methods of clinically successful neo-organs use a combination of decellularized donor organs, along with adult stem cells of the organ recipient to account for both the structural support of a donor organ and the personalization of the organ for each individual patient to reduce the chance of rejection.
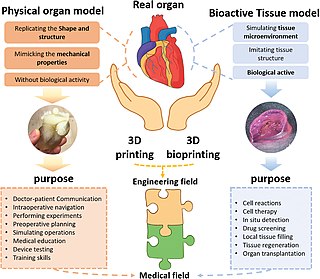
Three dimensional (3D) bioprinting is the utilization of 3D printing–like techniques to combine cells, growth factors, and/or biomaterials to fabricate biomedical parts, often with the aim of imitating natural tissue characteristics. Generally, 3D bioprinting can utilize a layer-by-layer method to deposit materials known as bio-inks to create tissue-like structures that are later used in various medical and tissue engineering fields. 3D bioprinting covers a broad range of bioprinting techniques and biomaterials. Currently, bioprinting can be used to print tissue and organ models to help research drugs and potential treatments. Nonetheless, translation of bioprinted living cellular constructs into clinical application is met with several issues due to the complexity and cell number needed to create functional organs. However, innovations span from bioprinting of extracellular matrix to mixing cells with hydrogels deposited layer by layer to produce the desired tissue. In addition, 3D bioprinting has begun to incorporate the printing of scaffolds. These scaffolds can be used to regenerate joints and ligaments.
Tengion, Inc. is an American development-stage regenerative medicine company founded in 2003 with financing from J&J Development Corporation, HealthCap and Oak Investment Partners, which is headquartered in Winston-Salem, North Carolina. Its goals are discovering, developing, manufacturing and commercializing a range of replacement organs and tissues, or neo-organs and neo-tissues, to address unmet medical needs in urologic, renal, gastrointestinal, and vascular diseases and disorders. The company creates these human neo-organs from a patient’s own cells or autologous cells, in conjunction with its Organ Regeneration Platform. The company declared Chapter 7 bankruptcy in December 2014, and it, along with its assets and tissue engineering samples, have been bought back by its creditors and former executives as of March 2015. The purchase was expedited, so that time-sensitive research can continue.
Genital regeneration encompasses various forms of treatment for genital anomalies. The goal of these treatments is to restore form and function to male and female genitalia by taking advantage of innate responses in the body. In order to do this, doctors have experimented with stem cells and extracellular matrix to provide a framework for regenerating missing structures. More research is needed to successfully move the science from laboratory trials to routine procedures.
Regeneration in humans is the regrowth of lost tissues or organs in response to injury. This is in contrast to wound healing, or partial regeneration, which involves closing up the injury site with some gradation of scar tissue. Some tissues such as skin, the vas deferens, and large organs including the liver can regrow quite readily, while others have been thought to have little or no capacity for regeneration following an injury.
References
- 1 2 "Treatments & Procedures", Urinary Reconstruction and Diversion, Cleveland Clinic , retrieved 2013-03-22
- 1 2 3 Atala A, Bauer SB, Soker S, Yoo JJ, Retik AB (April 2006). "Tissue-engineered autologous bladders for patients needing cystoplasty". Lancet. 367 (9518): 1241–6. doi:10.1016/S0140-6736(06)68438-9. PMID 16631879. S2CID 17892321.
- Lay summary in: Chung SY. "Bladder tissue-engineering: a new practical solution?".(subscription required)