Hypospadias is a common malformation in fetal development of the penis in which the urethra does not open from its usual location on the head of the penis. It is the second-most common birth defect of the male reproductive system, affecting about one of every 250 males at birth, although when including milder cases, is found in up to 4% of newborn males. Roughly 90% of cases are the less serious distal hypospadias, in which the urethral opening is on or near the head of the penis (glans). The remainder have proximal hypospadias, in which the meatus is all the way back on the shaft of the penis, near or within the scrotum. Shiny tissue or anything that typically forms the urethra instead extends from the meatus to the tip of the glans; this tissue is called the urethral plate.

An epispadias is a rare type of malformation in which the urethra ends, in males, in an opening on the upper aspect of the penis, and in females when the urethra develops too far anteriorly. It occurs in around 1 in 120,000 male and 1 in 500,000 female births.
Cloacal exstrophy (CE) is a severe birth defect wherein much of the abdominal organs are exposed. It often causes the splitting of the bladder, genitalia, and the anus. It is sometimes called OEIS complex.
Pediatric urology is a surgical subspecialty of medicine dealing with the disorders of children's genitourinary systems. Pediatric urologists provide care for both boys and girls ranging from birth to early adult age. The most common problems are those involving disorders of urination, reproductive organs and testes.

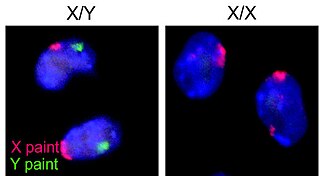
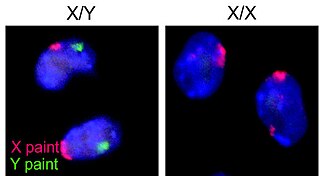
Intersex medical interventions (IMI), sometimes known as intersex genital mutilations (IGM), are surgical, hormonal and other medical interventions performed to modify atypical or ambiguous genitalia and other sex characteristics, primarily for the purposes of making a person's appearance more typical and to reduce the likelihood of future problems. The history of intersex surgery has been characterized by controversy due to reports that surgery can compromise sexual function and sensation, and create lifelong health issues. The medical interventions can be for a variety of reasons, due to the enormous variety of the disorders of sex development. Some disorders, such as salt-wasting disorder, can be life-threatening if left untreated.

The history of intersex surgery is intertwined with the development of the specialities of pediatric surgery, pediatric urology, and pediatric endocrinology, with our increasingly refined understanding of sexual differentiation, with the development of political advocacy groups united by a human qualified analysis, and in the last decade by doubts as to efficacy, and controversy over when and even whether some procedures should be performed.

Prostatectomy is the surgical removal of all or part of the prostate gland. This operation is done for benign conditions that cause urinary retention, as well as for prostate cancer and for other cancers of the pelvis.
Nocturia is defined by the International Continence Society (ICS) as "the complaint that the individual has to wake at night one or more times for voiding ". The term is derived from Latin nox – "night", and Greek [τα] ούρα – "urine". Causes are varied and can be difficult to discern. Although not every patient needs treatment, most people seek treatment for severe nocturia, waking up to void more than 2 or 3 times per night.
Urethroplasty is the surgical repair of an injury or defect within the walls of the urethra. Trauma, iatrogenic injury and infections are the most common causes of urethral injury/defect requiring repair. Urethroplasty is regarded as the gold standard treatment for urethral strictures and offers better outcomes in terms of recurrence rates than dilatations and urethrotomies. It is probably the only useful modality of treatment for long and complex strictures though recurrence rates are higher for this difficult treatment group.
Sacral nerve stimulation, also termed sacral neuromodulation, is a type of medical electrical stimulation therapy.
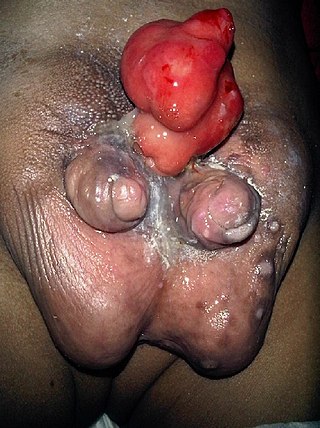
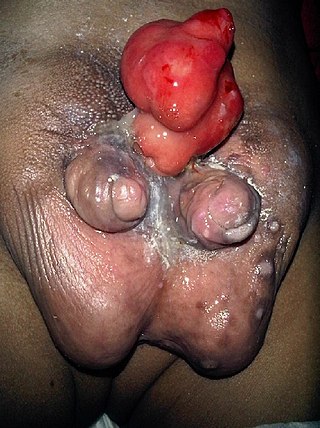
Diphallia, penile duplication (PD), diphallic terata, or diphallasparatus is an extremely rare developmental abnormality in which a male is born with two penises. The first reported case was by Johannes Jacob Wecker in 1609. Its occurrence is 1 in 5.5 million boys in the United States.
The mechanics of human sexuality or mechanics of sex, or more formally the biomechanics of human sexuality, is the study of the mechanics related to human sexual activity. Examples of topics include the biomechanical study of the strength of vaginal tissues and the biomechanics of male erectile function. The mechanics of sex under limit circumstances, such as sexual activity at zero-gravity in outer space, are also being studied.

Cystitis cystica is an uncommon chronic reactive inflammatory disease that is believed to be brought on by a tumor, calculi, infection, or obstruction of the urothelium. Cystitis glandularis is a proliferative progression of cystitis cystica that is distinguished by urothelial glandular metaplasia.

Buried penis, also called hidden penis or retractile penis, is a congenital or acquired condition in which the penis is partially or completely hidden below the surface of the skin. A buried penis can lead to urinary difficulties, poor hygiene, infection, and inhibition of normal sexual function.

Eosinophilic cystitis is a rare type of interstitial cystitis first reported in 1960 by Edwin Brown. Eosinophilic cystitis has been linked to a number of etiological factors, including allergies, bladder tumors, trauma to the bladder, parasitic infections, and chemotherapy drugs, though the exact cause of the condition is still unknown. The antigen-antibody response is most likely the cause of eosinophilic cystitis. This results in the generation of different immunoglobulins, which activate eosinophils and start the inflammatory process.

An artificial urinary sphincter (AUS) is an implanted device to treat moderate to severe stress urinary incontinence, most commonly in men. The AUS is designed to supplement the function of the natural urinary sphincter that restricts urine flow out of the bladder.
Male genital examination is a physical examination of the genital in males to detect ailments and to assess sexual development, and is normally a component of an annual physical examination. The examination includes checking the penis, scrotum, and urethral meatus. A comprehensive assessment of the male genitals assesses the pubic hair based on Sexual Maturity Rating and the size of the testicles and penis. The exam can also be conducted to verify a person's age and biological sex. The genitourinary system can also be assessed as part of the male genital examination. During a genital examination, the doctor can detect any of the following: structural abnormalities, urethral opening abnormalities, problems related to not being circumcised, lumps, tumors, redness, excoriation, edema, lesions, swelling, cancer, hair-related issues, and many others. In some instances where a physical examination of the male genitals is not sufficient to diagnose an individual, then an internal genital examination using imaging or ultrasounds will be needed for further evaluation.

Zephyr Surgical Implants (ZSI) is a Swiss-based medical device manufacturer that produces and distributes artificial urinary sphincters and penile implants worldwide. ZSI products are used in the management of moderate-to-severe urinary incontinence in men, erectile dysfunction, Peyronie's disease, penis enlargement, and female-to-male gender reassignment surgery.
Penile implants may be employed to treat erectile dysfunction or urinary troubles after a spinal cord injury.
William G. Reiner is a urologist, psychiatrist and professor who worked and taught at Johns Hopkins Hospital and University of Oklahoma. He researched individuals with intersex conditions, cloacal exstrophy and bladder exstrophy.