Related Research Articles

Caesarean section, also known as C-section, cesarean, or caesarean delivery, is the surgical procedure by which one or more babies are delivered through an incision in the mother's abdomen. It is often performed because vaginal delivery would put the mother or child at risk. Reasons for the operation include obstructed labor, twin pregnancy, high blood pressure in the mother, breech birth, shoulder presentation, and problems with the placenta or umbilical cord. A caesarean delivery may be performed based upon the shape of the mother's pelvis or history of a previous C-section. A trial of vaginal birth after C-section may be possible. The World Health Organization recommends that caesarean section be performed only when medically necessary.

Twins are two offspring produced by the same pregnancy. Twins can be either monozygotic ('identical'), meaning that they develop from one zygote, which splits and forms two embryos, or dizygotic, meaning that each twin develops from a separate egg and each egg is fertilized by its own sperm cell. Since identical twins develop from one zygote, they will share the same sex, while fraternal twins may or may not. In very rare cases twins can have the same mother and different fathers.
A multiple birth is the culmination of one multiple pregnancy, wherein the mother gives birth to two or more babies. A term most applicable to vertebrate species, multiple births occur in most kinds of mammals, with varying frequencies. Such births are often named according to the number of offspring, as in twins and triplets. In non-humans, the whole group may also be referred to as a litter, and multiple births may be more common than single births. Multiple births in humans are the exception and can be exceptionally rare in the largest mammals.

Childbirth, also known as labour, parturition and delivery, is the completion of pregnancy where one or more babies exits the internal environment of the mother via vaginal delivery or caesarean section. In 2019, there were about 140.11 million human births globally. In developed countries, most deliveries occur in hospitals, while in developing countries most are home births.

A breech birth is when a baby is born bottom first instead of head first, as is normal. Around 3–5% of pregnant women at term have a breech baby. Due to their higher than average rate of possible complications for the baby, breech births are generally considered higher risk. Breech births also occur in many other mammals such as dogs and horses, see veterinary obstetrics.
Labor induction is the process or treatment that stimulates childbirth and delivery. Inducing (starting) labor can be accomplished with pharmaceutical or non-pharmaceutical methods. In Western countries, it is estimated that one-quarter of pregnant women have their labor medically induced with drug treatment. Inductions are most often performed either with prostaglandin drug treatment alone, or with a combination of prostaglandin and intravenous oxytocin treatment.
A hysterotomy is an incision made in the uterus. This surgical incision is used in several medical procedures, including during termination of pregnancy in the second trimester and delivering the fetus during caesarean section. It is also used to gain access and perform surgery on a fetus during pregnancy to correct birth defects, and it is an option to achieve resuscitation if cardiac arrest occurs during pregnancy and it is necessary to remove the fetus from the uterus.
Prenatal perception is the study of the extent of somatosensory and other types of perception during pregnancy. In practical terms, this means the study of fetuses; none of the accepted indicators of perception are present in embryos. Studies in the field inform the abortion debate, along with certain related pieces of legislation in countries affected by that debate. As of 2022, there is no scientific consensus on whether a fetus can feel pain.

Chorioamnionitis, also known as amnionitis and intra-amniotic infection (IAI), is inflammation of the fetal membranes, usually due to bacterial infection. In 2015, a National Institute of Child Health and Human Development Workshop expert panel recommended use of the term "triple I" to address the heterogeneity of this disorder. The term triple I refers to intrauterine infection or inflammation or both and is defined by strict diagnostic criteria, but this terminology has not been commonly adopted although the criteria are used.

Fetal surgery, also known as antenatal surgery or prenatal surgery, is a growing branch of maternal-fetal medicine that covers any of a broad range of surgical techniques that are used to treat congenital abnormalities in fetuses who are still in the pregnant uterus. There are three main types: open fetal surgery, which involves completely opening the uterus to operate on the fetus; minimally invasive fetoscopic surgery, which uses small incisions and is guided by fetoscopy and sonography; and percutaneous fetal therapy, which involves placing a catheter under continuous ultrasound guidance.
Caesarean delivery on maternal request (CDMR) is a caesarean section birth requested by the pregnant woman without a medical reason.
In case of a previous caesarean section a subsequent pregnancy can be planned beforehand to be delivered by either of the following two main methods:
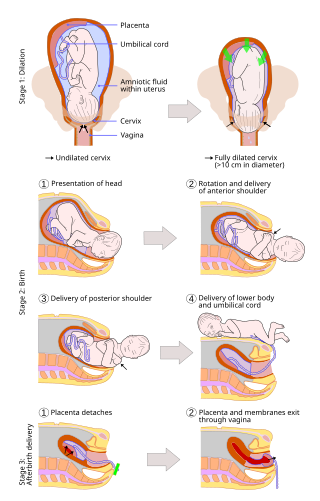
A vaginal delivery is the birth of offspring in mammals through the vagina. It is the most common method of childbirth worldwide. It is considered the preferred method of delivery, as it is correlated with lower morbidity and mortality than caesarean sections (C-sections), though it is not clear whether this is causal.
In obstetrics, asynclitic birth, or asynclitism, refers to the malposition of the fetal head in the uterus relative to the birth canal. Many babies enter the pelvis in an asynclitic presentation, but in most cases, it corrects itself spontaneously during labor. Asynclitic presentation is not to be confused with a shoulder presentation, where the shoulder leads first.

Velamentous cord insertion is a complication of pregnancy where the umbilical cord is inserted in the fetal membranes. It is a major cause of antepartum hemorrhage that leads to loss of fetal blood and associated with high perinatal mortality. In normal pregnancies, the umbilical cord inserts into the middle of the placental mass and is completely encased by the amniotic sac. The vessels are hence normally protected by Wharton's jelly, which prevents rupture during pregnancy and labor. In velamentous cord insertion, the vessels of the umbilical cord are improperly inserted in the chorioamniotic membrane, and hence the vessels traverse between the amnion and the chorion towards the placenta. Without Wharton's jelly protecting the vessels, the exposed vessels are susceptible to compression and rupture.
The following outline is provided as an overview of and topical guide to obstetrics:
Amnioinfusion is a method in which isotonic fluid is instilled into the uterine cavity.
The Human Microbiome Project (HMP), completed in 2012, laid the foundation for further investigation into the role the microbiome plays in overall health and disease. One area of particular interest is the role which delivery mode plays in the development of the infant/neonate microbiome and what potential implications this may have long term. It has been found that infants born via vaginal delivery have microbiomes closely mirroring that of the mother's vaginal microbiome, whereas those born via cesarean section tend to resemble that of the mother's skin. One notable study from 2010 illustrated an abundance of Lactobacillus and other typical vaginal genera in stool samples of infants born via vaginal delivery and an abundance of Staphylococcus and Corynebacterium, commonly found on the skin surfaces, in stool samples of infants born via cesarean section. From these discoveries came the concept of vaginal seeding, also known as microbirthing, which is a procedure whereby vaginal fluids are applied to a new-born child delivered by caesarean section. The idea of vaginal seeding was explored in 2015 after Maria Gloria Dominguez-Bello discovered that birth by caesarean section significantly altered the newborn child's microbiome compared to that of natural birth. The purpose of the technique is to recreate the natural transfer of bacteria that the baby gets during a vaginal birth. It involves placing swabs in the mother's vagina, and then wiping them onto the baby's face, mouth, eyes and skin. Due to the long-drawn nature of studying the impact of vaginal seeding, there are a limited number of studies available that support or refute its use. The evidence suggests that applying microbes from the mother's vaginal canal to the baby after cesarean section may aid in the partial restoration of the infant's natural gut microbiome with an increased likelihood of pathogenic infection to the child via vertical transmission.
Jennifer J. Kurinczuk is a British physician who is a Professor of Perinatal Epidemiology and Director of the National Perinatal Epidemiology Unit at the University of Oxford. In 2019 she was named an Honorary Fellow of the Royal College of Obstetricians and Gynaecologists. During the COVID-19 pandemic, Kurinczuk investigated the neonatal complications of coronavirus disease.
Women's rights in Djibouti are a source of concern for various human rights organizations, both within Djibouti and without. While minority groups are represented at all levels of the government, they effectively have no power to alter legislation, due to the repressive nature of the regime. Despite a legal quota that ensures that women hold at least 25 percent of the seats in the National Assembly, they remain underrepresented in leadership positions. Over 60% of women are illiterate. They face barriers to employment and appropriate health care. Rates of female genital mutilation remain high despite campaigns dating back to the 1980s.
References
- 1 2 3 "Australian Academy of Health and Medical Sciences - search term: Nicholas Fisk".
- ↑ "Prof. Nicholas Maxwell FISK". Who's Who Australia.
- ↑ Smith, J., Plaat, F., and Fisk, N.M. (2008). "The natural caesarean: A woman-centred technique". BJOG: An International Journal of Obstetrics and Gynaecology. 115 (8): 1037–1041
- ↑ "Every bit as magical". The Guardian. 3 December 2005.
- ↑ Capogna, G. and de Boer, H. (2017). "Humanization of Cesarean Section" In: Anesthesia for Cesarean Section. Cham: Springer International Publishing Switzerland. p. 185.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ↑ Armbrust, R., Hinkson, L. von Weizsacker, K., Henrich, W. (2016). "The Charite cesarean birth: a family orientated approach of cesarean section". The Journal of Maternal-Fetal & Neonatal Medicine. 29 (1): 163–168. doi:10.3109/14767058.2014.991917. PMID 25572878. S2CID 27558028.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Posthuma, S., Korteweg, F.J., van der Ploeg, J.M., de Boer, H.D., Buiter, H.D., and van der Ham, D.P. (2017). "Risks and benefits of the skin-to-skin cesarean section – a retrospective cohort study". The Journal of Maternal-Fetal & Neonatal Medicine. 30 (2): 159–163. doi:10.3109/14767058.2016.1163683. PMID 26955857. S2CID 24696681.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Narayen, I.C., Mulder, E.E.M., Boers, K.E., van Vonderen, J.J., Wolters, V.E.R.A., Freeman, L.M., and Te Pas, A.B. (2018). "Neonatal Safety of Elective Family-Centered Caesarean Sections: A Cohort Study". Frontiers in Pediatrics. 6 (20): 20. doi: 10.3389/fped.2018.00020 . PMC 5816568 . PMID 29484289.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Schorn, M.N., Moore, E., Spetalnick, B.M., and Morad, A (2015). "Implementing Family-Centred Cesarean Birth". Journal of Midwifery & Women's Health. 60 (6): 682–690. doi:10.1111/jmwh.12400. PMID 26618328.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ "ESA (European Society of Anaesthesiology). Natural Caesarean section is safe, popular and feasible and is not encouraging maternal requests for C-section births" Science Daily. 5 June 2017.
- ↑ "UNSW announces new Deputy Vice-Chancellor (Research)". UNSW Newsroom. 16 May 2016.
- ↑ Rosenthal, Elizabeth (4 April 2007). "A warehouse for stem cells offers hope for families, at a price". The New York Times.
- ↑ "Mother tells of 'horror' at giving birth to stillborn twins". The Independent (Ireland). 18 November 2004.
- ↑ Connor, Steve (30 July 2002). "Stem cell discovery raises prospect of treating genetic disorders in the womb" . The Independent (UK). Archived from the original on 18 June 2022.
- ↑ Stepney, Rob (18 February 1997). "The issue of foetal pain is being highlighted by anti-abortionists. But its implications extend beyond their agenda - to the process of birth itself" . The Independent (UK). Archived from the original on 18 June 2022.
- ↑ "Leading researcher to head clinical research centre". UQ News. 5 July 2007.
- ↑ "Professor Nicholas Fisk". Research Australia.
- ↑ "UQ Professor leaves Health in better shape". UQ News. 28 June 2009.
- ↑ "2001 Annual Meeting". International Fetal Medicine and Surgery Society (IFMSS). 2018.
- ↑ "International Fetal Medicine and Surgery Society - History". International Fetal Medicine and Surgery Society (IFMSS). 2018.
- ↑ "AAHC Board of Directors & AAHCI Steering Committee". Association of Academic Health Centers. 2018.
- ↑ "Nicholas Fisk Appointed AAHCI Steering Committee Chair and to AAHC Board of Directors". Globe Newswire. 5 July 2016.
- ↑ "NICHOLAS FISK APPOINTED AAHCI STEERING COMMITTEE CHAIR AND TO AAHC BOARD OF DIRECTORS". The Association of Academic Health Centers (AAHC). 2018.
- ↑ Fisk, Nicholas. "Professor" (PDF). Queen's Birthday 2020 Honours List.
- ↑ "Research Australia Board" . Retrieved 28 February 2022.
- ↑ Gabbett, Michael T.; Laporte, Johanna; Sekar, Renuka; Nandini, Adayapalam; McGrath, Pauline; Sapkota, Yadav; Jiang, Peiyong; Zhang, Haiqiang; Burgess, Trent (28 February 2019). "Molecular Support for Heterogonesis Resulting in Sesquizygotic Twinning". New England Journal of Medicine. 380 (9): 842–849. doi: 10.1056/NEJMoa1701313 . hdl: 10072/384437 . ISSN 0028-4793. PMID 30811910.
- ↑ Murphy, Heather (8 March 2019). "Congratulations, It's Twins. The Doctor Is Perplexed". The New York Times.
- ↑ Maxouris, Christina (1 March 2019). "Semi-identical twins are rare, and doctors say they've identified the second case ever". CNN.
- ↑ "Semi-identical twins 'identified for only the second time'". BBC News. 27 February 2019.
- ↑ "Nicholas M Fisk FAHMS FRSN PhD MBA MBBS FRCOG FRANZCOG CMFM DDU GAICD". Google Scholar.
- ↑ "In pictures: 'Natural caesarean'". BBC News. 20 December 2007.
- ↑ Balaskas, Janet (15 September 2014). "Planning for a 'Natural Caesarean'". Active Birth Centre.
- ↑ Philby, Charlotte (25 October 2015). "Natural caesarean: Why I chose a gentler version of the operation for my baby after two surgical births" . Independent. Archived from the original on 18 June 2022.
- ↑ Hendry, Joene (29 August 2008). ""Natural" cesarean mimics vaginal birth experience". Reuters Health.
- ↑ Phelps, Kerryn (21 March 2001). "The pros and cons of natural delivery and C-sections". Australian Medical Association.
- ↑ Revill, Jo (6 March 2006). "Why mothers should be offered caesareans".
- ↑ "The safest method of birth is by caesarean". 2 May 2004.
- ↑ Ronan, Alex (23 February 2017). "The Pro-Choice Movement has a Science Problem". The Outline.
- ↑ Dermer, Hon Ed (18 March 1998). "CRIMINAL CODE AMENDMENT (ABORTION) BILL - SECOND READING". Parliament of Western Australia.
- ↑ Towalski, Joe (21 April 2011). "Can an unborn child feel pain?". Catholic Hotdish.
- ↑ Agresti, James D (2 June 2015). "Media Promotes Junk Science on Fetal Pain". Crisis Magazine.
- ↑ Polman, Dick (22 July 2015). "Scott Walker Versus Science". The Moderate Voice.