Migraine is a genetically influenced complex neurological disorder characterized by episodes of moderate-to-severe headache, most often unilateral and generally associated with nausea and light and sound sensitivity. Other characterizing symptoms may include vomiting, cognitive dysfunction, allodynia, and dizziness. Exacerbation of headache symptoms during physical activity is another distinguishing feature. Up to one-third of migraine sufferers experience aura, a premonitory period of sensory disturbance widely accepted to be caused by cortical spreading depression at the onset of a migraine attack. Although primarily considered to be a headache disorder, migraine is highly heterogenous in its clinical presentation and is better thought of as a spectrum disease rather than a distinct clinical entity. Disease burden can range from episodic discrete attacks to chronic disease.
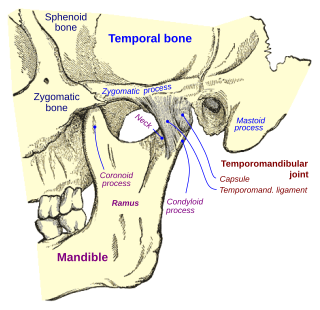
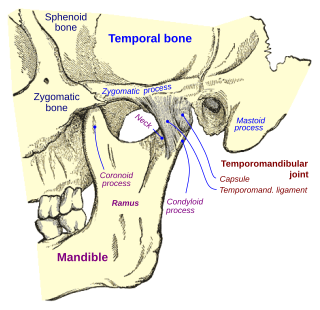
Temporomandibular joint dysfunction is an umbrella term covering pain and dysfunction of the muscles of mastication and the temporomandibular joints. The most important feature is pain, followed by restricted mandibular movement, and noises from the temporomandibular joints (TMJ) during jaw movement. Although TMD is not life-threatening, it can be detrimental to quality of life; this is because the symptoms can become chronic and difficult to manage.

Headache, also known as cephalalgia, is the symptom of pain in the face, head, or neck. It can occur as a migraine, tension-type headache, or cluster headache. There is an increased risk of depression in those with severe headaches.

Bruxism is excessive teeth grinding or jaw clenching. It is an oral parafunctional activity; i.e., it is unrelated to normal function such as eating or talking. Bruxism is a common behavior; reports of prevalence range from 8% to 31% in the general population. Several symptoms are commonly associated with bruxism, including aching jaw muscles, headaches, hypersensitive teeth, tooth wear, and damage to dental restorations. Symptoms may be minimal, without patient awareness of the condition. If nothing is done, after a while many teeth start wearing down until the whole tooth is gone.
Cluster headache is a neurological disorder characterized by recurrent severe headaches on one side of the head, typically around the eye(s). There is often accompanying eye watering, nasal congestion, or swelling around the eye on the affected side. These symptoms typically last 15 minutes to 3 hours. Attacks often occur in clusters which typically last for weeks or months and occasionally more than a year.
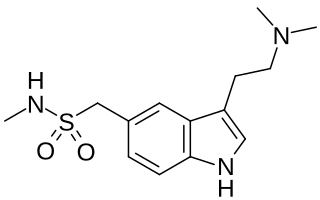
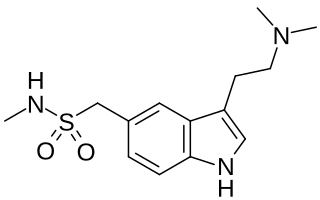
Triptans are a family of tryptamine-based drugs used as abortive medication in the treatment of migraines and cluster headaches. This drug class was first commercially introduced in the 1990s. While effective at treating individual headaches, they do not provide preventive treatment and are not considered a cure. They are not effective for the treatment of tension–type headache, except in persons who also experience migraines. Triptans do not relieve other kinds of pain.

A mouthguard is a protective device for the mouth that covers the teeth and gums to prevent and reduce injury to the teeth, arches, lips and gums. An effective mouthguard is like a crash helmet for teeth and jaws. It also prevents the jaws coming together fully, thereby reducing the risk of jaw joint injuries and concussion. A mouthguard is most often used to prevent injury in contact sports, as a treatment for bruxism or TMD, or as part of certain dental procedures, such as tooth bleaching or sleep apnea treatment. Depending on the application, it may also be called a mouth protector, mouth piece, gumshield, gumguard, nightguard, occlusal splint, bite splint, or bite plane. The dentists who specialise in sports dentistry fabricate mouthguards.
Neuralgia is pain in the distribution of a nerve or nerves, as in intercostal neuralgia, trigeminal neuralgia, and glossopharyngeal neuralgia.

Allodynia is a condition in which pain is caused by a stimulus that does not normally elicit pain. For example, sunburn can cause temporary allodynia, so that usually painless stimuli, such as wearing clothing or running cold or warm water over it, can be very painful. It is different from hyperalgesia, an exaggerated response from a normally painful stimulus. The term comes from Ancient Greek άλλος (állos) 'other', and οδύνη (odúnē) 'pain'.

Calcitonin gene-related peptide (CGRP) is a member of the calcitonin family of peptides consisting of calcitonin, amylin, adrenomedullin, adrenomedullin 2 (intermedin) and calcitonin‑receptor‑stimulating peptide. Calcitonin is mainly produced by thyroid C cells whilst CGRP is secreted and stored in the nervous system. This peptide, in humans, exists in two forms: CGRP alpha, and CGRP beta. α-CGRP is a 37-amino acid neuropeptide and is formed by alternative splicing of the calcitonin/CGRP gene located on chromosome 11. β-CGRP is less studied. In humans, β-CGRP differs from α-CGRP by three amino acids and is encoded in a separate, nearby gene. The CGRP family includes calcitonin (CT), adrenomedullin (AM), and amylin (AMY).

Dental attrition is a type of tooth wear caused by tooth-to-tooth contact, resulting in loss of tooth tissue, usually starting at the incisal or occlusal surfaces. Tooth wear is a physiological process and is commonly seen as a normal part of aging. Advanced and excessive wear and tooth surface loss can be defined as pathological in nature, requiring intervention by a dental practitioner. The pathological wear of the tooth surface can be caused by bruxism, which is clenching and grinding of the teeth. If the attrition is severe, the enamel can be completely worn away leaving underlying dentin exposed, resulting in an increased risk of dental caries and dentin hypersensitivity. It is best to identify pathological attrition at an early stage to prevent unnecessary loss of tooth structure as enamel does not regenerate.
Occlusion, in a dental context, means simply the contact between teeth. More technically, it is the relationship between the maxillary (upper) and mandibular (lower) teeth when they approach each other, as occurs during chewing or at rest.

Crossbite is a form of malocclusion where a tooth has a more buccal or lingual position than its corresponding antagonist tooth in the upper or lower dental arch. In other words, crossbite is a lateral misalignment of the dental arches.
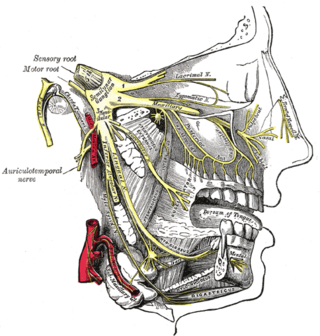
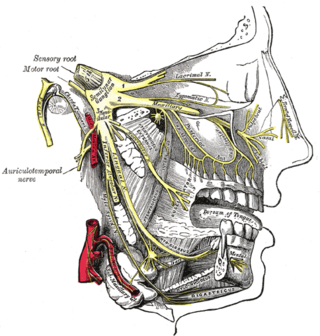
Migraine surgery is a surgical operation undertaken with the goal of reducing or preventing migraines. Migraine surgery most often refers to surgical nerve decompression of one or several nerves in the head and neck which have been shown to trigger migraine symptoms in many migraine sufferers. Following the development of nerve decompression techniques for the relief of migraine pain in the year 2000, these procedures have been extensively studied and shown to be effective in appropriate candidates. The nerves that are most often addressed in migraine surgery are found outside of the skull, in the face and neck, and include the supra-orbital and supra-trochlear nerves in the forehead, the zygomaticotemporal nerve and auriculotemporal nerves in the temple region, and the greater occipital, lesser occipital, and third occipital nerves in the back of the neck. Nerve impingement in the nasal cavity has additionally been shown to be a trigger of migraine symptoms.
Preventive treatment of migraine can be an important component of migraine management. The goals of preventive therapy are to reduce the frequency, painfulness, and/or duration of migraine attacks, and to increase the effectiveness of abortive therapy. Another reason to pursue prevention is to avoid medication overuse headache (MOH), otherwise known as rebound headache, which can arise from overuse of pain medications, and can result in chronic daily headache. Preventive treatments of migraine include medications, nutritional supplements, lifestyle alterations, and surgery. Prevention is recommended in those who have headaches more than two days a week, cannot tolerate the medications used to treat acute attacks, or those with severe attacks that are not easily controlled.
Short-lasting unilateral neuralgiform headache with conjunctival injection and tearing is a rare headache disorder that belongs to the group of headaches called trigeminal autonomic cephalalgia (TACs). Symptoms include excruciating burning, stabbing, or electrical headaches mainly near the eye and typically these sensations are only on one side of the body. The headache attacks are typically accompanied by cranial autonomic signs that are unique to SUNCT. Each attack can last from five seconds to six minutes and may occur up to 200 times daily.
Atypical facial pain (AFP) is a type of chronic facial pain which does not fulfill any other diagnosis. There is no consensus as to a globally accepted definition, and there is even controversy as to whether the term should be continued to be used. Both the International Headache Society (IHS) and the International Association for the Study of Pain (IASP) have adopted the term persistent idiopathic facial pain (PIFP) to replace AFP. In the 2nd Edition of the International Classification of Headache Disorders (ICHD-2), PIFP is defined as "persistent facial pain that does not have the characteristics of the cranial neuralgias ... and is not attributed to another disorder." However, the term AFP continues to be used by the World Health Organization's 10th revision of the International Statistical Classification of Diseases and Related Health Problems and remains in general use by clinicians to refer to chronic facial pain that does not meet any diagnostic criteria and does not respond to most treatments.
Dentomandibular sensorimotor dysfunction (DMSD) is a medical condition involving the mandible, upper three cervical (neck) vertebrae, and the surrounding muscle and nerve areas.

Orofacial pain is a general term covering any pain which is felt in the mouth, jaws and the face. Orofacial pain is a common symptom, and there are many causes.

Tooth mobility is the horizontal or vertical displacement of a tooth beyond its normal physiological boundaries around the gingival area, i.e. the medical term for a loose tooth.