Related Research Articles

An arteriovenous malformation (AVM) is an abnormal connection between arteries and veins, bypassing the capillary system. Usually congenital, this vascular anomaly is widely known because of its occurrence in the central nervous system, but can appear anywhere in the body. The symptoms of AVMs can range from none at all to intense pain or bleeding, and they can lead to other serious medical problems.

Veins are blood vessels in the circulatory system of humans and most other animals that carry blood towards the heart. Most veins carry deoxygenated blood from the tissues back to the heart; exceptions are those of the pulmonary and fetal circulations which carry oxygenated blood to the heart. In the systemic circulation, arteries carry oxygenated blood away from the heart, and veins return deoxygenated blood to the heart, in the deep veins.

Heart murmurs are unique heart sounds produced when blood flows across a heart valve or blood vessel. This occurs when turbulent blood flow creates a sound loud enough to hear with a stethoscope. The sound differs from normal heart sounds by their characteristics. For example, heart murmurs may have a distinct pitch, duration and timing. The major way health care providers examine the heart on physical exam is heart auscultation; another clinical technique is palpation, which can detect by touch when such turbulence causes the vibrations called cardiac thrill. A murmur is a sign found during the cardiac exam. Murmurs are of various types and are important in the detection of cardiac and valvular pathologies.

Tetralogy of Fallot (TOF), formerly known as Steno-Fallot tetralogy, is a congenital heart defect characterized by four specific cardiac defects. Classically, the four defects are:

Interventional radiology (IR) is a medical specialty that performs various minimally-invasive procedures using medical imaging guidance, such as x-ray fluoroscopy, computed tomography, magnetic resonance imaging, or ultrasound. IR performs both diagnostic and therapeutic procedures through very small incisions or body orifices. Diagnostic IR procedures are those intended to help make a diagnosis or guide further medical treatment, and include image-guided biopsy of a tumor or injection of an imaging contrast agent into a hollow structure, such as a blood vessel or a duct. By contrast, therapeutic IR procedures provide direct treatment—they include catheter-based medicine delivery, medical device placement, and angioplasty of narrowed structures.
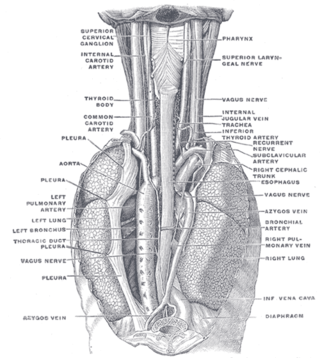
The azygos vein is a vein running up the right side of the thoracic vertebral column draining itself towards the superior vena cava. It connects the systems of superior vena cava and inferior vena cava and can provide an alternative path for blood to the right atrium when either of the venae cavae is blocked.
A cyanotic heart defect is any congenital heart defect (CHD) that occurs due to deoxygenated blood bypassing the lungs and entering the systemic circulation, or a mixture of oxygenated and unoxygenated blood entering the systemic circulation. It is caused by structural defects of the heart such as right-to-left or bidirectional shunting, malposition of the great arteries, or any condition which increases pulmonary vascular resistance. The result may be the development of collateral circulation.
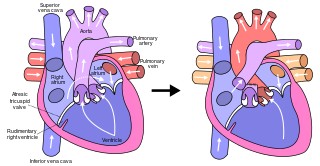
The Fontan procedure or Fontan–Kreutzer procedure is a palliative surgical procedure used in children with univentricular hearts. It involves diverting the venous blood from the inferior vena cava (IVC) and superior vena cava (SVC) to the pulmonary arteries. The procedure varies for differing congenital heart pathologies. For example, in tricuspid atresia, the procedure can be done where the blood does not pass through the morphologic right ventricle; i.e., the systemic and pulmonary circulations are placed in series with the functional single ventricle. By contrast, in hypoplastic left heart syndrome, the heart is more reliant on the more functional right ventricle to provide blood flow to the systemic circulation. The procedure was initially performed in 1968 by Francis Fontan and Eugene Baudet from Bordeaux, France, published in 1971, simultaneously described in July 1971 by Guillermo Kreutzer from Buenos Aires, Argentina, presented at the Argentinean National Cardilogy meeting of that year and finally published in 1973.
A transthoracic echocardiogram (TTE) is the most common type of echocardiogram, which is a still or moving image of the internal parts of the heart using ultrasound. In this case, the probe is placed on the chest or abdomen of the subject to get various views of the heart. It is used as a non-invasive assessment of the overall health of the heart, including a patient's heart valves and degree of heart muscle contraction. The images are displayed on a monitor for real-time viewing and then recorded.

Scimitar syndrome, or congenital pulmonary venolobar syndrome, is a rare congenital heart defect characterized by anomalous venous return from the right lung. This anomalous pulmonary venous return can be either partial (PAPVR) or total (TAPVR). The syndrome associated with PAPVR is more commonly known as Scimitar syndrome after the curvilinear pattern created on a chest radiograph by the pulmonary veins that drain to the inferior vena cava. This radiographic density often has the shape of a scimitar, a type of curved sword. The syndrome was first described by Catherine Neill in 1960.
A right-to-left shunt is a cardiac shunt which allows blood to flow from the right heart to the left heart. This terminology is used both for the abnormal state in humans and for normal physiological shunts in reptiles.

Subclavian steal syndrome (SSS), also called subclavian steal steno-occlusive disease, is a medical condition characterized by retrograde (reversed) blood flow in the vertebral artery or the internal thoracic artery. This reversal occurs due to proximal stenosis (narrowing) or occlusion of the subclavian artery.
In cardiology, a cardiac shunt is a pattern of blood flow in the heart that deviates from the normal circuit of the circulatory system. It may be described as right-left, left-right or bidirectional, or as systemic-to-pulmonary or pulmonary-to-systemic. The direction may be controlled by left and/or right heart pressure, a biological or artificial heart valve or both. The presence of a shunt may also affect left and/or right heart pressure either beneficially or detrimentally.

The bidirectional Glenn (BDG) shunt, or bidirectional cavopulmonary anastomosis, is a surgical technique used in pediatric cardiac surgery procedure used to temporarily improve blood oxygenation for patients with a congenital cardiac defect resulting in a single functional ventricle. Creation of a bidirectional shunt reduces the amount of blood volume that the heart needs to pump at the time of surgical repair with the Fontan procedure.
The Kawashima procedure is used for congenital heart disease with a single effective ventricle and an interrupted inferior vena cava (IVC). It was first performed in 1978 and reported in 1984.
Vascular myelopathy refers to an abnormality of the spinal cord in regard to its blood supply. The blood supply is complicated and supplied by two major vessel groups: the posterior spinal arteries and the anterior spinal arteries—of which the Artery of Adamkiewicz is the largest. Both the posterior and anterior spinal arteries run the entire length of the spinal cord and receive anastomotic (conjoined) vessels in many places. The anterior spinal artery has a less efficient supply of blood and is therefore more susceptible to vascular disease. Whilst atherosclerosis of spinal arteries is rare, necrosis in the anterior artery can be caused by disease in vessels originating from the segmental arteries such as atheroma or aortic dissection.

Hypoplastic right heart syndrome (HRHS) is a congenital heart defect in which the structures on the right side of the heart, particularly the right ventricle, are underdeveloped. This defect causes inadequate blood flow to the lungs, and thus a cyanotic infant.

Vein of Galen aneurysmal malformations(VGAMs) and Vein of Galen aneurysmal dilations (VGADs) are the most frequent arteriovenous malformations in infants and fetuses. A VGAM consists of a tangled mass of dilated vessels supplied by an enlarged artery. The malformation increases greatly in size with age, although the mechanism of the increase is unknown. Dilation of the great cerebral vein of Galen is a secondary result of the force of arterial blood either directly from an artery via an arteriovenous fistula or by way of a tributary vein that receives the blood directly from an artery. There is usually a venous anomaly downstream from the draining vein that, together with the high blood flow into the great cerebral vein of Galen causes its dilation. The right sided cardiac chambers and pulmonary arteries also develop mild to severe dilation.
The Senning procedure is an atrial switch heart operation performed to treat transposition of the great arteries. It is named after its inventor, the Swedish cardiac surgeon Åke Senning (1915–2000), also known for implanting the first permanent cardiac pacemaker in 1958.
Isolated levocardia is a rare type of organs' situs inversus in which the heart is still in normal position but other abdominal viscera are transposed. Isolated levocardia may occur with heart defects and patients without having operations have low life expectancy: only about 5% to 13% of patients survive more than 5 years. Therefore, even though the risk of cardiac surgeries is high, once patients are diagnosed, operations are suggested to be held as soon as possible. Isolated levocardia is congenital. So far, there is not sufficient evidence to prove that chromosome abnormalities will result in isolated levocardia, and the cause of isolated levocardia is still unknown.
References
- ↑ LearningRadiology.com > Coarctation Of the Aorta Retrieved August 2010
- ↑ "Medcyclopaedia - Rib notching" . Retrieved 2010-04-15.