Ambulatory care or outpatient care is medical care provided on an outpatient basis, including diagnosis, observation, consultation, treatment, intervention, and rehabilitation services. This care can include advanced medical technology and procedures even when provided outside of hospitals.
A dietitian, medical dietitian, or dietician is an expert in identifying and treating disease-related malnutrition and in conducting medical nutrition therapy, for example designing an enteral tube feeding regimen or mitigating the effects of cancer cachexia. Many dietitians work in hospitals and usually see specific patients where a nutritional assessment and intervention has been requested by a doctor or nurse, for example if a patient has lost their ability to swallow or requires artificial nutrition due to intestinal failure. Dietitians are regulated healthcare professionals licensed to assess, diagnose, and treat such problems. In the United Kingdom, dietitian is a 'protected title', meaning identifying yourself as a dietitian without appropriate education and registration is prohibited by law.
The Sociedade Brasileira de Informática em Saúde, abbreviated as SBIS, is a professional society created in November 1986 in Campinas, during the First Brazilian Congress on Health Informatics. It has the mission of promoting the development and the interchange of ideas and results in the fields devoted to the information technologies applied to the health sciences.

Telehealth is the distribution of health-related services and information via electronic information and telecommunication technologies. It allows long-distance patient and clinician contact, care, advice, reminders, education, intervention, monitoring, and remote admissions. Telemedicine is sometimes used as a synonym, or is used in a more limited sense to describe remote clinical services, such as diagnosis and monitoring. When rural settings, lack of transport, a lack of mobility, conditions due to outbreaks, epidemics or pandemics, decreased funding, or a lack of staff restrict access to care, telehealth may bridge the gap as well as provide distance-learning; meetings, supervision, and presentations between practitioners; online information and health data management and healthcare system integration. Telehealth could include two clinicians discussing a case over video conference; a robotic surgery occurring through remote access; physical therapy done via digital monitoring instruments, live feed and application combinations; tests being forwarded between facilities for interpretation by a higher specialist; home monitoring through continuous sending of patient health data; client to practitioner online conference; or even videophone interpretation during a consult.

Telenursing refers to the use of information technology in the provision of nursing services whenever physical distance exists between patient and nurse, or between any number of nurses. As a field, it is part of telemedicine, and has many points of contacts with other medical and non-medical applications, such as telediagnosis, teleconsultation, and telemonitoring. The field, however, is still being developed as the information on telenursing isn't comprehensive enough.
A licensed practical nurse (LPN), in much of the United States and Canada, is a nurse who cares for people who are sick, injured, convalescent, or disabled. In the United States, LPNs work under the direction of physicians, mid-level practitioners, and may work under the direction of registered nurses depending on their jurisdiction.

A nurse practitioner (NP) is an advanced practice registered nurse and a type of mid-level practitioner. NPs are trained to assess patient needs, order and interpret diagnostic and laboratory tests, diagnose disease, formulate and prescribe medications and treatment plans. NP training covers basic disease prevention, coordination of care, and health promotion, but does not provide the depth of expertise needed to recognize more complex conditions.
Telepsychiatry is the application of telemedicine to the specialty field of psychiatry. The term typically describes the delivery of psychiatric assessment and care through telecommunications technology, usually videoconferencing. Telepsychiatry services can be offered through intermediary companies that partner with facilities to increase care capacities, or by individual providers or provider groups. Most commonly, telepsychiatry encounters take place at medical facilities under the supervision of onsite staff, though at-home models are becoming accepted as long as they are in compliance with HIPAA standards.

In medicine, rural health or rural medicine is the interdisciplinary study of health and health care delivery in rural environments. The concept of rural health incorporates many fields, including geography, midwifery, nursing, sociology, economics, and telehealth or telemedicine.
Home automation for the elderly and disabled focuses on making it possible for older adults and people with disabilities to remain at home, safe and comfortable. Home automation is becoming a viable option for older adults and people with disabilities who would prefer to stay in the comfort of their homes rather than move to a healthcare facility. This field uses much of the same technology and equipment as home automation for security, entertainment, and energy conservation but tailors it towards old people and people with disabilities.

Nursing is a profession within the health care sector focused on the care of individuals, families, and communities so they may attain, maintain, or recover optimal health and quality of life. They also take on vital roles of education, assessing situations, as support. Nurses may be differentiated from other health care providers by their approach to patient care, training, and scope of practice. Nurses practice in many specialties with differing levels of prescription authority. Nurses comprise the largest component of most healthcare environments; but there is evidence of international shortages of qualified nurses. Many nurses provide care within the ordering scope of physicians, and this traditional role has shaped the public image of nurses as care providers. Nurse practitioners are nurses with a graduate degree in advanced practice nursing. They are however permitted by most jurisdictions to practice independently in a variety of settings. Since the postwar period, nurse education has undergone a process of diversification towards advanced and specialized credentials, and many of the traditional regulations and provider roles are changing.
Ambulatory care nursing is the nursing care of patients who receive treatment on an outpatient basis, ie they do not require admission to a hospital for an overnight stay. Ambulatory care includes those clinical, organizational and professional activities engaged in by registered nurses with and for individuals, groups, and populations who seek assistance with improving health and/or seek care for health-related problems. The American Academy of Ambulatory Care Nursing (AAACN) describes ambulatory care nursing as a comprehensive practice which is built on a broad knowledge base of nursing and health sciences, and applies clinical expertise rooted in the nursing process.

A health facility is, in general, any location where healthcare is provided. Health facilities range from small clinics and doctor's offices to urgent care centers and large hospitals with elaborate emergency rooms and trauma centers. The number and quality of health facilities in a country or region is one common measure of that area's prosperity and quality of life. In many countries, health facilities are regulated to some extent by law; licensing by a regulatory agency is often required before a facility may open for business. Health facilities may be owned and operated by for-profit businesses, non-profit organizations, governments, and in some cases by individuals, with proportions varying by country. See also the recent review paper,
Connected health is a socio-technical model for healthcare management and delivery by using technology to provide healthcare services remotely. Connected health, also known as technology enabled care (TEC) aims to maximize healthcare resources and provide increased, flexible opportunities for consumers to engage with clinicians and better self-manage their care. It uses readily available consumer technologies to deliver patient care outside of the hospital or doctor's office. Connected health encompasses programs in telehealth, remote care and disease and lifestyle management, often leverages existing technologies such as connected devices using cellular networks and is associated with efforts to improve chronic care. However, there is an increasing blur between software capabilities and healthcare needs whereby technologists are now providing the solutions to support consumer wellness and provide the connectivity between patient data, information and decisions. This calls for new techniques to guide Connected Health solutions such as "design thinking" to support software developers in clearly identifying healthcare requirements, and extend and enrich traditional software requirements gathering techniques.
Unlicensed assistive personnel (UAP) are paraprofessionals who assist individuals with physical disabilities, mental impairments, and other health care needs with their activities of daily living (ADLs). UAPs also provide bedside care—including basic nursing procedures—all under the supervision of a registered nurse, licensed practical nurse or other health care professional. UAPs must demonstrate their ability and competence before gaining any expanded responsibilities in a clinical setting. While providing this care, UAPs offer compassion and patience and are part of the patient's healthcare support system. Communication between UAPs and registered nurses (RNs) is key as they are working together in their patients' best interests. The scope of care UAPs are responsible for is delegated by RNs or other clinical licensed professionals.

Telehomecare (THC) is a subfield within telehealth. It involves the delivery of healthcare services to patients at home through the use of telecommunications technologies, which enable the interaction of voice, video, and health-related data. The management of care is done from an external site by a healthcare professional.
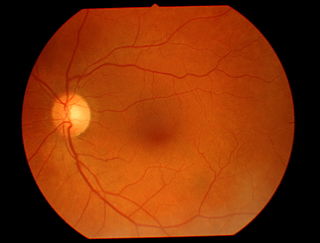
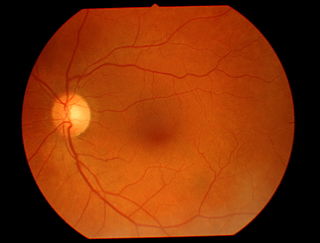
Teleophthalmology is a branch of telemedicine that delivers eye care through digital medical equipment and telecommunications technology. Today, applications of teleophthalmology encompass access to eye specialists for patients in remote areas, ophthalmic disease screening, diagnosis and monitoring; as well as distant learning.

Telepharmacy is the delivery of pharmaceutical care via telecommunications to patients in locations where they may not have direct contact with a pharmacist. It is an instance of the wider phenomenon of telemedicine, as implemented in the field of pharmacy. Telepharmacy services include drug therapy monitoring, patient counseling, prior authorization and refill authorization for prescription drugs, and monitoring of formulary compliance with the aid of teleconferencing or videoconferencing. Remote dispensing of medications by automated packaging and labeling systems can also be thought of as an instance of telepharmacy. Telepharmacy services can be delivered at retail pharmacy sites or through hospitals, nursing homes, or other medical care facilities.
Credentialing is the process of establishing the qualifications of licensed medical professionals and assessing their background and legitimacy.

Peter Yellowlees is a British-born American physician, researcher, academic and administrator. He is Chief Wellness Officer at UC Davis Health and Distinguished Professor of General Psychiatry at University of California, Davis. He holds the Alan Stoudemire Endowed Chair in Psychiatry and is the Director of Physician Health Program at UC Davis Psychiatry. He chairs the UCDH Wellbeing Committee.