An analgesic drug, also called simply an analgesic, pain reliever, or painkiller, is any member of the group of drugs used to achieve relief from pain. Analgesics are conceptually distinct from anesthetics, which temporarily reduce, and in some instances eliminate, sensation, although analgesia and anesthesia are neurophysiologically overlapping and thus various drugs have both analgesic and anesthetic effects.

Chiropractic is a form of alternative medicine concerned with the diagnosis, treatment and prevention of mechanical disorders of the musculoskeletal system, especially of the spine. It has esoteric origins and is based on several pseudoscientific ideas.

Ketamine is a dissociative anesthetic used medically for induction and maintenance of anesthesia. It is also used as a treatment for depression, and as a pain management tool. Ketamine is a novel compound that was derived from phencyclidine in 1962 in pursuit of a safer anesthetic with fewer hallucinogenic effects.
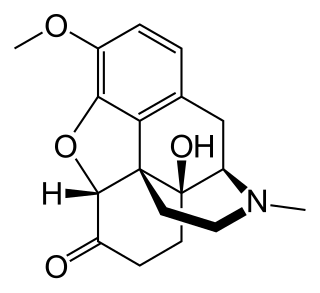
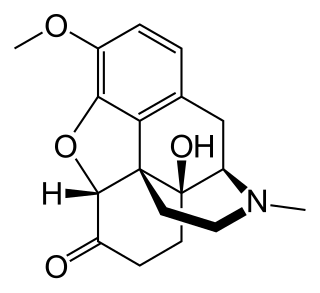
Oxycodone, sold under various brand names such as Roxicodone and OxyContin, is a semi-synthetic opioid used medically for treatment of moderate to severe pain. It is highly addictive and is a commonly abused drug. It is usually taken by mouth, and is available in immediate-release and controlled-release formulations. Onset of pain relief typically begins within fifteen minutes and lasts for up to six hours with the immediate-release formulation. In the United Kingdom, it is available by injection. Combination products are also available with paracetamol (acetaminophen), ibuprofen, naloxone, naltrexone, and aspirin.

Pain is a distressing feeling often caused by intense or damaging stimuli. The International Association for the Study of Pain defines pain as "an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage."
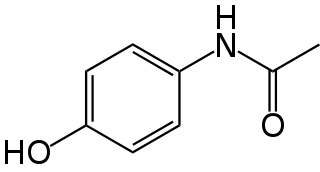
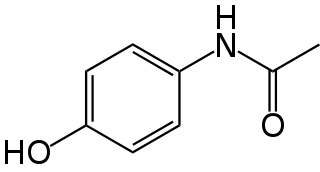
Paracetamol is a non-opioid analgesic and antipyretic agent used to treat fever and mild to moderate pain. It is a widely used over the counter medication and common brand names include Tylenol and Panadol.
Chronic pain is classified as pain that lasts longer than three months. In medicine, the distinction between acute and chronic pain is sometimes determined by the amount of time since onset. Two commonly used markers are pain that continues at three months and six months since onset, but some theorists and researchers have placed the transition from acute to chronic pain at twelve months. Others apply the term acute to pain that lasts less than 30 days, chronic to pain of more than six months duration, and subacute to pain that lasts from one to six months. A popular alternative definition of chronic pain, involving no fixed duration, is "pain that extends beyond the expected period of healing".
Palliative care is an interdisciplinary medical caregiving approach aimed at optimizing quality of life and mitigating suffering among people with serious, complex, and often terminal illnesses. Within the published literature, many definitions of palliative care exist. The World Health Organization (WHO) describes palliative care as "an approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial, and spiritual". In the past, palliative care was a disease specific approach, but today the WHO takes a broader patient-centered approach that suggests that the principles of palliative care should be applied as early as possible to any chronic and ultimately fatal illness. This shift was important because if a disease-oriented approach is followed, the needs and preferences of the patient are not fully met and aspects of care, such as pain, quality of life, and social support, as well as spiritual and emotional needs, fail to be addressed. Rather, a patient-centered model prioritizes relief of suffering and tailors care to increase the quality of life for terminally ill patients.

Trigeminal neuralgia, also called Fothergill disease, tic douloureux, trifacial neuralgia, or suicide disease is a long-term pain disorder that affects the trigeminal nerve, the nerve responsible for sensation in the face and motor functions such as biting and chewing. It is a form of neuropathic pain. There are two main types: typical and atypical trigeminal neuralgia. The typical form results in episodes of severe, sudden, shock-like pain in one side of the face that lasts for seconds to a few minutes. Groups of these episodes can occur over a few hours. The atypical form results in a constant burning pain that is less severe. Episodes may be triggered by any touch to the face. Both forms may occur in the same person. It is regarded as one of the most painful disorders known to medicine, and often results in depression and suicide.
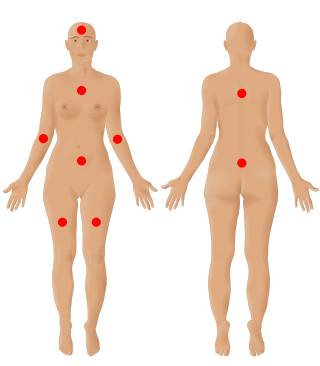
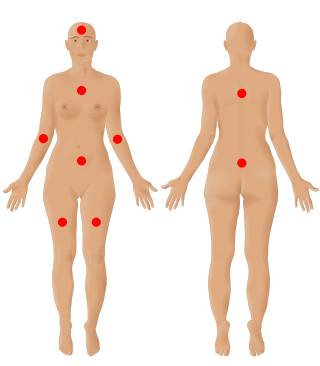
Fibromyalgia is a medical condition defined by the presence of chronic widespread pain, fatigue, waking unrefreshed, cognitive symptoms, lower abdominal pain or cramps, and depression. Other symptoms include insomnia and a general hypersensitivity.

Pain management is an aspect of medicine and health care involving relief of pain in various dimensions, from acute and simple to chronic and challenging. Most physicians and other health professionals provide some pain control in the normal course of their practice, and for the more complex instances of pain, they also call on additional help from a specific medical specialty devoted to pain, which is called pain medicine.

Gabapentin, sold under the brand name Neurontin among others, is an anticonvulsant medication primarily used to treat partial seizures and neuropathic pain. It is commonly used medication for the treatment of neuropathic pain caused by diabetic neuropathy, postherpetic neuralgia, and central pain. It is moderately effective: about 30–40% of those given gabapentin for diabetic neuropathy or postherpetic neuralgia have a meaningful benefit.

Osteoarthritis (OA) is a type of degenerative joint disease that results from breakdown of joint cartilage and underlying bone. It is believed to be the fourth leading cause of disability in the world, affecting 1 in 7 adults in the United States alone. The most common symptoms are joint pain and stiffness. Usually the symptoms progress slowly over years. Other symptoms may include joint swelling, decreased range of motion, and, when the back is affected, weakness or numbness of the arms and legs. The most commonly involved joints are the two near the ends of the fingers and the joint at the base of the thumbs, the knee and hip joints, and the joints of the neck and lower back. The symptoms can interfere with work and normal daily activities. Unlike some other types of arthritis, only the joints, not internal organs, are affected.

Opioids are a class of drugs that derive from, or mimic, natural substances found in the opium poppy plant. Opioids work in the brain to produce a variety of effects, including pain relief. As a class of substances, they act on opioid receptors to produce morphine-like effects.

Buprenorphine, sold under the brand name Subutex among others, is an opioid used to treat opioid use disorder, acute pain, and chronic pain. It can be used under the tongue (sublingual), in the cheek (buccal), by injection, as a skin patch (transdermal), or as an implant. For opioid use disorder, it is typically started when withdrawal symptoms have begun and for the first two days of treatment under direct observation of a health-care provider.

Plantar fasciitis or plantar heel pain is a disorder of the plantar fascia, which is the connective tissue which supports the arch of the foot. It results in pain in the heel and bottom of the foot that is usually most severe with the first steps of the day or following a period of rest. Pain is also frequently brought on by bending the foot and toes up towards the shin. The pain typically comes on gradually, and it affects both feet in about one-third of cases.
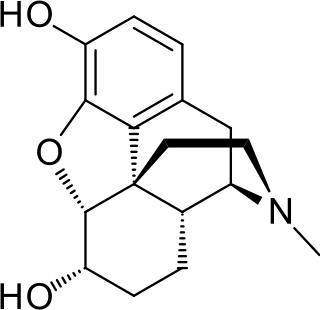
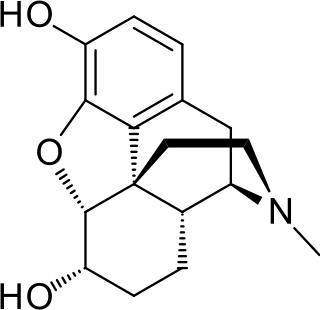
Dihydromorphine is a semi-synthetic opioid structurally related to and derived from morphine. The 7,8-double bond in morphine is reduced to a single bond to get dihydromorphine. Dihydromorphine is a moderately strong analgesic and is used clinically in the treatment of pain and also is an active metabolite of the analgesic opioid drug dihydrocodeine. Dihydromorphine occurs in trace quantities in assays of opium on occasion, as does dihydrocodeine, dihydrothebaine, tetrahydrothebaine, etc. The process for manufacturing dihydromorphine from morphine for pharmaceutical use was developed in Germany in the late 19th century, with the synthesis being published in 1900 and the drug introduced clinically as Paramorfan shortly thereafter. A high-yield synthesis from tetrahydrothebaine was later developed.

Orofacial pain is a general term covering any pain which is felt in the mouth, jaws and the face. Orofacial pain is a common symptom, and there are many causes.

M. R. Rajagopal is an Indian palliative care physician (anesthesiologist) and professor referred to as the 'father of palliative care in India' in honour of his significant contribution to the palliative care scene in India.

Prudence Margaret Burch, known professionally as Vidyamala Burch, is a mindfulness teacher, writer, and co-founder of Breathworks, an international mindfulness organization known particularly for developing mindfulness-based pain management (MBPM). The British Pain Society has recognized her "outstanding contribution to the alleviation of pain", and in 2019, 2020, 2021 and 2022 she was named on the Shaw Trust Power 100 list of the most influential disabled people in the UK. Burch's book Mindfulness for Health won the British Medical Association's 2014 Medical Books Award in the Popular Medicine category.