Related Research Articles
A mental disorder, also referred to as a mental illness or psychiatric disorder, is a behavioral or mental pattern that causes significant distress or impairment of personal functioning. A mental disorder is also characterized by a clinically significant disturbance in an individual’s cognition, emotional regulation, or behaviour. It is usually associated with distress or impairment in important areas of functioning. There are many different types of mental disorders. Mental disorders may also be referred to as mental health conditions. Such features may be persistent, relapsing and remitting, or occur as single episodes. Many disorders have been described, with signs and symptoms that vary widely between specific disorders. Such disorders may be diagnosed by a mental health professional, usually a clinical psychologist or psychiatrist.
Anti-psychiatry is a movement based on the view that psychiatric treatment is often more damaging than helpful to patients, highlighting controversies about psychiatry. Objections include the reliability of psychiatric diagnosis, the questionable effectiveness and harm associated with psychiatric medications, the failure of psychiatry to demonstrate any disease treatment mechanism for psychiatric medication effects, and legal concerns about equal human rights and civil freedom being nullified by the presence of diagnosis. Historically critiques of psychiatry came to light after focus on the extreme harms associated with electroconvulsive treatment or insulin shock therapy. The term "anti-psychiatry" is in dispute and often used to dismiss all critics of psychiatry, many of who agree that a specialized role of helper for people in emotional distress may at times be appropriate, and allow for individual choice around treatment decisions.

Mental health encompasses emotional, psychological, and social well-being, influencing cognition, perception, and behavior. It likewise determines how an individual handles stress, interpersonal relationships, and decision-making. Mental health includes subjective well-being, perceived self-efficacy, autonomy, competence, intergenerational dependence, and self-actualization of one's intellectual and emotional potential, among others. From the perspectives of positive psychology or holism, mental health may include an individual's ability to enjoy life and to create a balance between life activities and efforts to achieve psychological resilience. Cultural differences, subjective assessments, and competing professional theories all affect how one defines "mental health". Some early signs related to mental health difficulties are sleep irritation, lack of energy, lack of appetite and thinking of harming yourself or others.

Suicide prevention is a collection of efforts to reduce the risk of suicide. Suicide is often preventable, and the efforts to prevent it may occur at the individual, relationship, community, and society level. Suicide is a serious public health problem that can have long-lasting effects on individuals, families, and communities. Preventing suicide requires strategies at all levels of society. This includes prevention and protective strategies for individuals, families, and communities. Suicide can be prevented by learning the warning signs, promoting prevention and resilience, and committing to social change.
Mental disorders are classified as a psychological condition marked primarily by sufficient disorganization of personality, mind, and emotions to seriously impair the normal psychological and often social functioning of the individual. Individuals diagnosed with certain mental disorders can be unable to function normally in society. Mental disorders may consist of several affective, behavioral, cognitive and perceptual components. The acknowledgement and understanding of mental health conditions has changed over time and across cultures. There are still variations in the definition, classification, and treatment of mental disorders.
Sigmund Freud postulated that women were more prone to neurosis because they experienced aggression towards the self, which stemmed from developmental issues. Freud's postulation is countered by the idea that societal factors, such as gender roles, may play a major role in the development of mental illness. When considering gender and mental illness, one must look to both biology and social/cultural factors to explain areas in which men and women are more likely to develop different mental illnesses. A patriarchal society, gender roles, personal identity, social media, and exposure to other mental health risk factors have adverse effects on the psychological perceptions of both men and women.
Medical model is the term coined by psychiatrist R. D. Laing in his The Politics of the Family and Other Essays (1971), for the "set of procedures in which all doctors are trained". It includes complaint, history, physical examination, ancillary tests if needed, diagnosis, treatment, and prognosis with and without treatment.
Assertive community treatment (ACT) is an intensive and highly integrated approach for community mental health service delivery. ACT teams serve individuals who have been diagnosed with serious and persistent forms of mental illness, predominantly but not exclusively the schizophrenia spectrum disorders. ACT service recipients may also have diagnostic profiles that include features typically found in other DSM-5 categories. Many have histories of frequent psychiatric hospitalization, substance abuse, victimization and trauma, arrests and incarceration, homelessness, and additional significant challenges. The symptoms and complications of their mental illnesses have led to serious functioning difficulties in several areas of life, often including work, social relationships, residential independence, money management, and physical health and wellness. By the time they start receiving ACT services, they are likely to have experienced failure, discrimination, and stigmatization, and their hope for the future is likely to be quite low.
The psychiatric survivors movement is a diverse association of individuals who either currently access mental health services, or who are survivors of interventions by psychiatry.
Psychiatric rehabilitation, also known as psych social rehabilitation, and sometimes simplified to psych rehab by providers, is the process of restoration of community functioning and well-being of an individual diagnosed in mental health or emotional disorder and who may be considered to have a psychiatric disability.
The recovery model, recovery approach or psychological recovery is an approach to mental disorder or substance dependence that emphasizes and supports a person's potential for recovery. Recovery is generally seen in this model as a personal journey rather than a set outcome, and one that may involve developing hope, a secure base and sense of self, supportive relationships, empowerment, social inclusion, coping skills, and meaning. Recovery sees symptoms as a continuum of the norm rather than an aberration and rejects sane-insane dichotomy.
Mental health literacy has been defined as "knowledge and beliefs about mental disorders which aid their recognition, management and prevention. Mental health literacy includes the ability to recognize specific disorders; knowing how to seek mental health information; knowledge of risk factors and causes, of self-treatments, and of professional help available; and attitudes that promote recognition and appropriate help-seeking". The concept of mental health literacy was derived from health literacy, which aims to increase patient knowledge about physical health, illnesses, and treatments.
The Critical Psychiatry Network (CPN) is a psychiatric organization based in the United Kingdom. It was created by a group of British psychiatrists who met in Bradford, England in January 1999 in response to proposals by the British government to amend the Mental Health Act 1983. They expressed concern about the implications of the proposed changes for human rights and the civil liberties of people with mental health illness. Most people associated with the group are practicing consultant psychiatrists in the United Kingdom's National Health Service (NHS), among them Dr Joanna Moncrieff. A number of non-consultant grade and trainee psychiatrists are also involved in the network.

The Kraepelinian dichotomy is the division of the major endogenous psychoses into the disease concepts of dementia praecox, which was reformulated as schizophrenia by Eugen Bleuler by 1908, and manic-depressive psychosis, which has now been reconceived as bipolar disorder. This division was formally introduced in the sixth edition of Emil Kraepelin's psychiatric textbook Psychiatrie. Ein Lehrbuch für Studirende und Aerzte, published in 1899. It has been highly influential on modern psychiatric classification systems, the DSM and ICD, and is reflected in the taxonomic separation of schizophrenia from affective psychosis. However, there is also a diagnosis of schizoaffective disorder to cover cases that seem to show symptoms of both.
IPS Supported Employment is an evidence-based approach to supported employment for people who have a mental illness. IPS stands for Individual Placement and Support. IPS supports people in their efforts to achieve steady, meaningful employment in mainstream competitive jobs, either part-time or full-time. This stands in contrast to other vocational rehabilitation approaches that employ people in sheltered workshops and other set-aside jobs.
Mental illnesses, also known as psychiatric disorders, are often inaccurately portrayed in the media. Films, television programs, books, magazines, and news programs often stereotype the mentally ill as being violent or unpredictable, unlike the great majority of the actual mentally ill. As a result, some of the public stigmatize the mentally ill and believe that the mentally ill should be shunned, locked away in mental institutions, heavily medicated, or a combination of the three. However, not only are most of those with psychiatric disorders able to function adequately in society, but many are able to work successfully and make substantial contributions to society.

Posttraumatic stress disorder (PTSD) is a cognitive disorder, which may occur after a traumatic event. It is a psychiatric disorder, which may occur across athletes at all levels of sport participation.

The Attribution Questionnaire (AQ) is a 27-item self-report assessment tool designed to measure public stigma towards people with mental illnesses. It assesses emotional reaction and discriminatory responses based on answers to a hypothetical vignette about a man with schizophrenia named Harry. There are several different versions of the vignette that test multiple forms of attribution. Responses assessing stigma towards Harry are in the form of 27 items rated on a Likert scale ranging from 1 (not at all) to 9 (very much). There are 9 subscales within the AQ that breakdown the responses one could have towards a person with mental illness into different categories. The AQ was created in 2003 by Dr. Patrick Corrigan and colleagues and has since been revised into smaller tests because of the complexity and hypothetical that did not capture children and adolescent's stigmas well. The later scales are the Attribution Questionnaire-9 (AQ-9), the revised Attribution Questionnaire (r-AQ), and the children's Attribution Questionnaire (AQ-8-C).
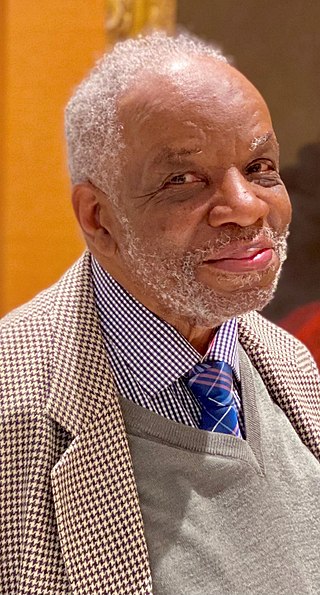
Aggrey Washington Burke is a British retired psychiatrist and academic, born in Jamaica, who spent the majority of his medical career at St George's Hospital in London, UK, specialising in transcultural psychiatry and writing literature on changing attitudes towards black people and mental health. He has carried out extensive research on racism and mental illness and is the first black consultant psychiatrist appointed by Britain's National Health Service (NHS).
Serious mental illness or severe mental illness (SMI) is characterized as any mental health condition that seriously impairs anywhere from one to several significant life activities including day to day functioning. Common diagnoses associated with SMI include bipolar disorder, psychotic disorders, post-traumatic stress disorder, and major depressive disorder. People experiencing SMI experience symptoms that can prevent them from having successful experiences that contribute to a good quality of life, due to social, physical, and psychological limitations of their illnesses. In 2017, there was a 4.5% prevalence rate of U.S. adults diagnosed with SMI, the highest percentage being the young adult population. In 2017, 66.7% of the 4.5% diagnosed adults sought out mental health care services.
References
- ↑ "Google Image Result for https://www.guilford.com/authors/photos/Corrigan_Patrick_W._95067.jpg". www.google.com. Retrieved 2022-05-02.
{{cite web}}: External link in|title= - ↑ www.mifellowship.org
- ↑ In 2022, Corrigan was awarded the 2022 American Psychological Association (APA) Award for Distinguished Contributions to Psychology in the Public Interest (Senior Career).www.mooddisorderscanada.ca Archived 2007-09-30 at the Wayback Machine
- ↑ www.mifellowship.org
- ↑ www.iit.edu
- ↑ www.amazon.com Dont-Call-Me-Nuts-Illness
- ↑ www.stigmaresearch.org Archived 2007-09-30 at archive.today
- ↑ Corrigan, Patrick W. (November 2020). "Challenges to welcoming people with mental illnesses into faith communities". The British Journal of Psychiatry. 217 (5): 595–596. doi: 10.1192/bjp.2020.83 . ISSN 0007-1250. PMID 32349817.
- ↑ Corrigan, Patrick W. (April 2016). "Resolving mental illness stigma: Should we seek normalcy or solidarity?". British Journal of Psychiatry. 208 (4): 314–315. doi: 10.1192/bjp.bp.115.169664 . ISSN 0007-1250. PMID 27036695.
- ↑ "Books by Patrick W Corrigan | Book Depository". www.bookdepository.com. Retrieved 2022-05-02.