Related Research Articles

Ascites is the abnormal build-up of fluid in the abdomen. Technically, it is more than 25 ml of fluid in the peritoneal cavity, although volumes greater than one liter may occur. Symptoms may include increased abdominal size, increased weight, abdominal discomfort, and shortness of breath. Complications can include spontaneous bacterial peritonitis.
In medicine, a shunt is a hole or a small passage that moves, or allows movement of, fluid from one part of the body to another. The term may describe either congenital or acquired shunts; acquired shunts may be either biological or mechanical.

The portal vein or hepatic portal vein (HPV) is a blood vessel that carries blood from the gastrointestinal tract, gallbladder, pancreas and spleen to the liver. This blood contains nutrients and toxins extracted from digested contents. Approximately 75% of total liver blood flow is through the portal vein, with the remainder coming from the hepatic artery proper. The blood leaves the liver to the heart in the hepatic veins.

Budd–Chiari syndrome is a very rare condition, affecting one in a million adults. The condition is caused by occlusion of the hepatic veins that drain the liver. It presents with the classical triad of abdominal pain, ascites, and liver enlargement. The formation of a blood clot within the hepatic veins can lead to Budd–Chiari syndrome. The syndrome can be fulminant, acute, chronic, or asymptomatic. Subacute presentation is the most common form.

Portal hypertension is abnormally increased portal venous pressure – blood pressure in the portal vein and its branches, that drain from most of the intestine to the liver. Portal hypertension is defined as a hepatic venous pressure gradient greater than 5 mmHg. Cirrhosis is the most common cause of portal hypertension; other, less frequent causes are therefore grouped as non-cirrhotic portal hypertension. When it becomes severe enough to cause symptoms or complications, treatment may be given to decrease portal hypertension itself or to manage its complications.
Situs ambiguus is a rare congenital defect in which the major visceral organs are distributed abnormally within the chest and abdomen. Clinically Heterotaxy spectrum generally refers to any defect of left-right laterality and arrangement of the visceral organs, however Classical Heterotaxy requires multiple organs to be affected. This does not include the congenital defect situs inversus, which results when arrangement of all the organs in the abdomen and chest are mirrored, so the positions are opposite the normal placement. Situs inversus is the mirror image of situs solitus, which is normal asymmetric distribution of the abdominothoracic visceral organs. Situs ambiguus can also be subdivided into left-isomerism and right isomerism based on the defects observed in the spleen, lungs and atria of the heart.

Hepatic encephalopathy (HE) is an altered level of consciousness as a result of liver failure. Its onset may be gradual or sudden. Other symptoms may include movement problems, changes in mood, or changes in personality. In the advanced stages it can result in a coma.

Hepatorenal syndrome is a life-threatening medical condition that consists of rapid deterioration in kidney function in individuals with cirrhosis or fulminant liver failure. HRS is usually fatal unless a liver transplant is performed, although various treatments, such as dialysis, can prevent advancement of the condition.

In the fetus, the ductus venosus shunts a portion of umbilical vein blood flow directly to the inferior vena cava. Thus, it allows oxygenated blood from the placenta to bypass the liver. Compared to the 50% shunting of umbilical blood through the ductus venosus found in animal experiments, the degree of shunting in the human fetus under physiological conditions is considerably less, 30% at 20 weeks, which decreases to 18% at 32 weeks, suggesting a higher priority of the fetal liver than previously realized. In conjunction with the other fetal shunts, the foramen ovale and ductus arteriosus, it plays a critical role in preferentially shunting oxygenated blood to the fetal brain. It is a part of fetal circulation.

Transjugular intrahepatic portosystemic shunt is an artificial channel within the liver that establishes communication between the inflow portal vein and the outflow hepatic vein. It is used to treat portal hypertension which frequently leads to intestinal bleeding, life-threatening esophageal bleeding and the buildup of fluid within the abdomen (ascites).

Portal vein thrombosis (PVT) is a vascular disease of the liver that occurs when a blood clot occurs in the hepatic portal vein, which can lead to increased pressure in the portal vein system and reduced blood supply to the liver. The mortality rate is approximately 1 in 10.

Gastric antral vascular ectasia (GAVE) is an uncommon cause of chronic gastrointestinal bleeding or iron deficiency anemia. The condition is associated with dilated small blood vessels in the pyloric antrum, which is a distal part of the stomach. The dilated vessels result in intestinal bleeding. It is also called watermelon stomach because streaky long red areas that are present in the stomach may resemble the markings on watermelon.

In medicine, a distal splenorenal shunt procedure (DSRS), also splenorenal shunt procedure and Warren shunt, is a surgical procedure in which the distal splenic vein is attached to the left renal vein. It is used to treat portal hypertension and its main complication. It was developed by W. Dean Warren.
A portacaval shunt is a treatment for portal hypertension. A connection is made between the portal vein, which supplies 75% of the liver's blood, and the inferior vena cava, the vein that drains blood from the lower two-thirds of the body. The most common causes of liver disease resulting in portal hypertension are Budd–Chiari Syndrome or Cirrhosis. Budd–Chiari should not be mistaken for Cirrhosis.

Portal hypertensive gastropathy refers to changes in the mucosa of the stomach in patients with portal hypertension; by far the most common cause of this is cirrhosis of the liver. These changes in the mucosa include friability of the mucosa and the presence of ectatic blood vessels at the surface. Patients with portal hypertensive gastropathy may experience bleeding from the stomach, which may uncommonly manifest itself in vomiting blood or melena; however, portal hypertension may cause several other more common sources of upper gastrointestinal bleeding, such as esophageal varices and gastric varices. On endoscopic evaluation of the stomach, this condition shows a characteristic mosaic or "snake-skin" appearance to the mucosa of the stomach.
Hepatic arterial infusion (HAI) is a medical procedure that delivers chemotherapy directly to the liver. The procedure, mostly used in combination with systemic chemotherapy, plays a role in the treatment of liver metastases in patients with colorectal cancer (CRC). Although surgical resection remains the standard of care for these liver metastases, majority of patients have lesions that are unresectable.

Selective internal radiation therapy (SIRT), also known as transarterial radioembolization (TARE), radioembolization or intra-arterial microbrachytherapy is a form of radiation therapy used in interventional radiology to treat cancer. It is generally for selected patients with surgically unresectable cancers, especially hepatocellular carcinoma or metastasis to the liver. The treatment involves injecting tiny microspheres of radioactive material into the arteries that supply the tumor, where the spheres lodge in the small vessels of the tumor. Because this treatment combines radiotherapy with embolization, it is also called radioembolization. The chemotherapeutic analogue is called chemoembolization, of which transcatheter arterial chemoembolization (TACE) is the usual form.
Anorectal varices are the dilation of collateral submucosal vessels due to backflow in the veins of the rectum. Typically this occurs due to portal hypertension which shunts venous blood from the portal system through the portosystemic anastomosis present at this site into the systemic venous system. This can also occur in the esophagus, causing esophageal varices, and at the level of the umbilicus, causing caput medusae. Between 44% and 78% of patients with portal hypertension get anorectal varices.
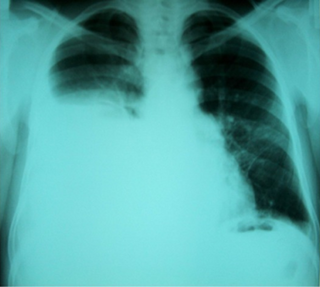
Hepatic hydrothorax is a rare form of pleural effusion that occurs in people with liver cirrhosis. It is defined as an effusion of over 500 mL in people with liver cirrhosis that is not caused by heart, lung, or pleural disease. It is found in 5-10% of people with liver cirrhosis and 2-3% of people with pleural effusions. It is much more common on the right side, with 85% of cases occurring on the right, 13% on the left, and 2% in both. Although it is most common in people with severe ascites, cases have been reported where people only had mild or no ascites. Symptoms are not specific, and mostly involve the respiratory system.
Congenital portosystemic shunts (PSS) is a hereditary condition in dogs and cats, its frequency varying depending on the breed. The shunts found mainly in small dog breeds such as Shih Tzus, Tibetan Spaniels, Miniature Schnauzers and Yorkshire Terriers, and in cats such as Persians, British Shorthairs, Himalayans, and mixed breeds are usually extrahepatic, while the shunts found in large dog breeds such as Irish Wolfhounds and Labrador Retrievers tend to be intrahepatic.
References
- ↑ Alonso-Gamarra, Eduardo; Parrón, Manuel; Pérez, Ana; Prieto, Consuelo; Hierro, Loreto; López-Santamaría, Manuel (2011-05-01). "Clinical and Radiologic Manifestations of Congenital Extrahepatic Portosystemic Shunts: A Comprehensive Review". RadioGraphics. 31 (3): 707–722. doi:10.1148/rg.313105070. ISSN 0271-5333. PMID 21571652.
- 1 2 3 4 Bernard, O.; Franchi-Abella, S.; Branchereau, S.; Pariente, D.; Gauthier, F.; Jacquemin, E. (November 2012). "Congenital Portosystemic Shunts in Children: Recognition, Evaluation, and Management". Seminars in Liver Disease. 32 (4): 273–287. doi: 10.1055/s-0032-1329896 . ISSN 0272-8087. PMID 23397528.
- 1 2 Papamichail, M.; Pizanias, M.; Heaton, N. (2018-03-01). "Congenital portosystemic venous shunt". European Journal of Pediatrics. 177 (3): 285–294. doi:10.1007/s00431-017-3058-x. ISSN 1432-1076. PMC 5816775 . PMID 29243189.
- 1 2 Stringer, Mark D. (2008). "The clinical anatomy of congenital portosystemic venous shunts". Clinical Anatomy. 21 (2): 147–157. doi:10.1002/ca.20574. ISSN 1098-2353. PMID 18161055. S2CID 42632424.
- 1 2 "Interview d'Amaria Remil, Cheffe de projet du Centre de Référence AVB-CG, et du Pr Stéphanie Franchi-Abella, Responsable du secteur de radiologie interventionnelle pédiatrique (Université Paris-Saclay)". Filfoie: tout savoir sur les maladies rares du foie, recherche, enseignement (in French). 2020-12-17. Retrieved 2021-07-28.
- 1 2 McLin, Valérie A.; Franchi Abella, Stephanie; Debray, Dominique; Guérin, Florent; Beghetti, Maurice; Savale, Laurent; Wildhaber, Barbara E.; Gonzales, Emmanuel; Members of the International Registry of Congenital Porto-Systemic Shunts (May 2019). "Congenital Portosystemic Shunts: Current Diagnosis and Management". Journal of Pediatric Gastroenterology and Nutrition. 68 (5): 615–622. doi:10.1097/MPG.0000000000002263. ISSN 1536-4801. PMID 30628988.
- ↑ Baiges, Anna; Turon, Fanny; Simón‐Talero, Macarena; Tasayco, Stephanie; Bueno, Javier; Zekrini, Kamal; Plessier, Aurélie; Franchi‐Abella, Stéphanie; Guerin, Florent; Mukund, Amar; Eapen, C.E. (February 2020). "Congenital Extrahepatic Portosystemic Shunts (Abernethy Malformation): An International Observational Study". Hepatology. 71 (2): 658–669. doi:10.1002/hep.30817. ISSN 0270-9139.
- ↑ Bahadori, Atessa; Kuhlmann, Beatrice; Debray, Dominique; Franchi-Abella, Stephanie; Wacker, Julie; Beghetti, Maurice; Wildhaber, Barbara E.; McLin, Valérie Anne; On Behalf Of The Ircpss, null (2022-02-11). "Presentation of Congenital Portosystemic Shunts in Children". Children. 9 (2): 243. doi: 10.3390/children9020243 . ISSN 2227-9067. PMC 8870378 . PMID 35204963.
- ↑ the International Registry of Congenital Portosystemic Shunt members; Franchi-Abella, Stéphanie; Gonzales, Emmanuel; Ackermann, Oanez; Branchereau, Sophie; Pariente, Danièle; Guérin, Florent (August 2018). "Congenital portosystemic shunts: diagnosis and treatment". Abdominal Radiology. 43 (8): 2023–2036. doi:10.1007/s00261-018-1619-8. ISSN 2366-004X. PMID 29730740. S2CID 19116849.
- ↑ McLin, Valérie; Franchi-Abella, S.; Debray, D.; Korff, S.; Casotti V; Colledan, M.; d'Antiga, L.; de Ville de Goyet, J.; Lurz, E.; Stéphenne, Xavier; Rock, Nathalie (2019). "Congenital porto-systemic shunts in children: preliminary results from the IRCPSS".
{{cite journal}}: Cite journal requires|journal=(help) - ↑ "Oral Abstracts (Abstracts 1–288)". Hepatology. 70 (S1): 1–187. October 2019. doi:10.1002/hep.30940. ISSN 0270-9139. S2CID 242005271.