Meconium aspiration syndrome (MAS) also known as neonatal aspiration of meconium is a medical condition affecting newborn infants. It describes the spectrum of disorders and pathophysiology of newborns born in meconium-stained amniotic fluid (MSAF) and have meconium within their lungs. Therefore, MAS has a wide range of severity depending on what conditions and complications develop after parturition. Furthermore, the pathophysiology of MAS is multifactorial and extremely complex which is why it is the leading cause of morbidity and mortality in term infants.

Meconium is the earliest stool of a mammalian infant resulting from defecation. Unlike later feces, meconium is composed of materials ingested during the time the infant spends in the uterus: intestinal epithelial cells, lanugo, mucus, amniotic fluid, bile, and water. Meconium, unlike later feces, is viscous and sticky like tar – its color usually being a very dark olive green and it is almost odorless. When diluted in amniotic fluid, it may appear in various shades of green, brown, or yellow. It should be completely passed by the end of the first few days after birth, with the stools progressing toward yellow.
Intrauterine growth restriction (IUGR), or fetal growth restriction, is the poor growth of a fetus while in the womb during pregnancy. IUGR is defined by clinical features of malnutrition and evidence of reduced growth regardless of an infant's birth weight percentile. The causes of IUGR are broad and may involve maternal, fetal, or placental complications.

Amniocentesis is a medical procedure used primarily in the prenatal diagnosis of genetic conditions. It has other uses such as in the assessment of infection and fetal lung maturity. Prenatal diagnostic testing, which includes amniocentesis, is necessary to conclusively diagnose the majority of genetic disorders, with amniocentesis being the gold-standard procedure after 15 weeks' gestation.
Fetal distress, also known as non-reassuring fetal status, is a condition during pregnancy or labor in which the fetus shows signs of inadequate oxygenation. Due to its imprecision, the term "fetal distress" has fallen out of use in American obstetrics. The term "non-reassuring fetal status" has largely replaced it. It is characterized by changes in fetal movement, growth, heart rate, and presence of meconium stained fluid.
Oligohydramnios is a medical condition in pregnancy characterized by a deficiency of amniotic fluid, the fluid that surrounds the fetus in the abdomen, in the amniotic sac. The limiting case is anhydramnios, where there is a complete absence of amniotic fluid. It is typically diagnosed by ultrasound when the amniotic fluid index (AFI) measures less than 5 cm or when the single deepest pocket (SDP) of amniotic fluid measures less than 2 cm. Amniotic fluid is necessary to allow for normal fetal movement, lung development, and cushioning from uterine compression. Low amniotic fluid can be attributed to a maternal, fetal, placental or idiopathic cause and can result in poor fetal outcomes including death. The prognosis of the fetus is dependent on the etiology, gestational age at diagnosis, and the severity of the oligohydramnios.

Twin-to-twin transfusion syndrome (TTTS), also known as feto-fetal transfusion syndrome (FFTS), twin oligohydramnios-polyhydramnios sequence (TOPS) and stuck twin syndrome, is a complication of monochorionic multiple pregnancies in which there is disproportionate blood supply between the fetuses. This leads to unequal levels of amniotic fluid between each fetus and usually leads to death of the undersupplied twin and, without treatment, usually death or a range of birth defects or disabilities for a surviving twin, such as underdeveloped, damaged or missing limbs, digits or organs, especially cerebral palsy.
Potter sequence is the atypical physical appearance of a baby due to oligohydramnios experienced when in the uterus. It includes clubbed feet, pulmonary hypoplasia and cranial anomalies related to the oligohydramnios. Oligohydramnios is the decrease in amniotic fluid volume sufficient to cause deformations in morphogenesis of the baby.
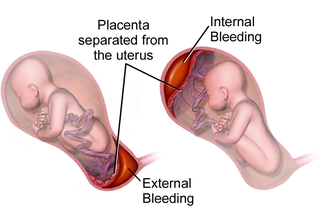
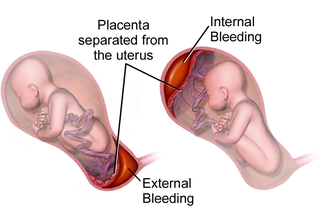
Placental abruption is when the placenta separates early from the uterus, in other words separates before childbirth. It occurs most commonly around 25 weeks of pregnancy. Symptoms may include vaginal bleeding, lower abdominal pain, and dangerously low blood pressure. Complications for the mother can include disseminated intravascular coagulopathy and kidney failure. Complications for the baby can include fetal distress, low birthweight, preterm delivery, and stillbirth.
In obstetrics, gestational age is a measure of the age of a pregnancy taken from the beginning of the woman's last menstrual period (LMP), or the corresponding age of the gestation as estimated by a more accurate method, if available. Such methods include adding 14 days to a known duration since fertilization, or by obstetric ultrasonography. The popularity of using this measure of pregnancy is largely due to convenience: menstruation is usually noticed, while there is generally no convenient way to discern when fertilization or implantation occurred.

Large for gestational age (LGA) is a term used to describe infants that are born with an abnormally high weight, specifically in the 90th percentile or above, compared to other babies of the same developmental age. Macrosomia is a similar term that describes excessive birth weight, but refers to an absolute measurement, regardless of gestational age. Typically the threshold for diagnosing macrosomia is a body weight between 4,000 and 4,500 grams, or more, measured at birth, but there are difficulties reaching a universal agreement of this definition.

Prelabor rupture of membranes (PROM), previously known as premature rupture of membranes, is breakage of the amniotic sac before the onset of labour. Women usually experience a painless gush or a steady leakage of fluid from the vagina. Complications in the baby may include premature birth, cord compression, and infection. Complications in the mother may include placental abruption and postpartum endometritis.

Complications of pregnancy are health problems that are related to, or arise during pregnancy. Complications that occur primarily during childbirth are termed obstetric labor complications, and problems that occur primarily after childbirth are termed puerperal disorders. While some complications improve or are fully resolved after pregnancy, some may lead to lasting effects, morbidity, or in the most severe cases, maternal or fetal mortality.

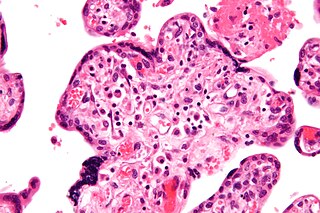
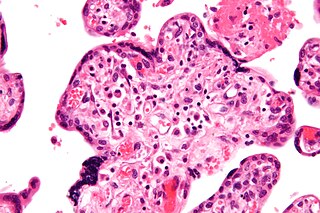
Chorioamnionitis, also known as amnionitis and intra-amniotic infection (IAI), is inflammation of the fetal membranes, usually due to bacterial infection. In 2015, a National Institute of Child Health and Human Development Workshop expert panel recommended use of the term "triple I" to address the heterogeneity of this disorder. The term triple I refers to intrauterine infection or inflammation or both and is defined by strict diagnostic criteria, but this terminology has not been commonly adopted although the criteria are used.
Postterm pregnancy is when a woman has not yet delivered her baby after 42 weeks of gestation, two weeks beyond the typical 40-week duration of pregnancy. Postmature births carry risks for both the mother and the baby, including fetal malnutrition, meconium aspiration syndrome, and stillbirths. After the 42nd week of gestation, the placenta, which supplies the baby with nutrients and oxygen from the mother, starts aging and will eventually fail. Postterm pregnancy is a reason to induce labor.

Circumvallate placenta is a rare condition affecting about 1-2% of pregnancies, in which the amnion and chorion fetal membranes essentially "double back" on the fetal side around the edges of the placenta. After delivery, a circumvallate placenta has a thick ring of membranes on its fetal surface. Circumvallate placenta is a placental morphological abnormality associated with increased fetal morbidity and mortality due to the restricted availability of nutrients and oxygen to the developing fetus.
Amnioinfusion is a method in which isotonic fluid is instilled into the uterine cavity.
Birth injury refers to damage or injury to the child before, during, or just after the birthing process. "Birth trauma" refers specifically to mechanical damage sustained during delivery.

Prenatal nutrition addresses nutrient recommendations before and during pregnancy. Nutrition and weight management before and during pregnancy has a profound effect on the development of infants. This is a rather critical time for healthy development since infants rely heavily on maternal stores and nutrient for optimal growth and health outcome later in life.
The anomaly scan, also sometimes called the anatomy scan, 20-week ultrasound, or level 2 ultrasound, evaluates anatomic structures of the fetus, placenta, and maternal pelvic organs. This scan is an important and common component of routine prenatal care. The function of the ultrasound is to measure the fetus so that growth abnormalities can be recognized quickly later in pregnancy, to assess for congenital malformations and multiple pregnancies, and to plan method of delivery.