Related Research Articles
In molecular biology, restriction fragment length polymorphism (RFLP) is a technique that exploits variations in homologous DNA sequences, known as polymorphisms, populations, or species or to pinpoint the locations of genes within a sequence. The term may refer to a polymorphism itself, as detected through the differing locations of restriction enzyme sites, or to a related laboratory technique by which such differences can be illustrated. In RFLP analysis, a DNA sample is digested into fragments by one or more restriction enzymes, and the resulting restriction fragments are then separated by gel electrophoresis according to their size.
A microsatellite is a tract of repetitive DNA in which certain DNA motifs are repeated, typically 5–50 times. Microsatellites occur at thousands of locations within an organism's genome. They have a higher mutation rate than other areas of DNA leading to high genetic diversity. Microsatellites are often referred to as short tandem repeats (STRs) by forensic geneticists and in genetic genealogy, or as simple sequence repeats (SSRs) by plant geneticists.
A genetic screen or mutagenesis screen is an experimental technique used to identify and select individuals who possess a phenotype of interest in a mutagenized population. Hence a genetic screen is a type of phenotypic screen. Genetic screens can provide important information on gene function as well as the molecular events that underlie a biological process or pathway. While genome projects have identified an extensive inventory of genes in many different organisms, genetic screens can provide valuable insight as to how those genes function.
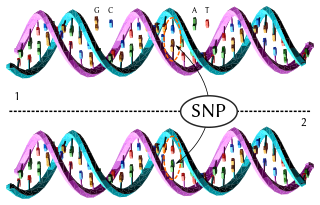
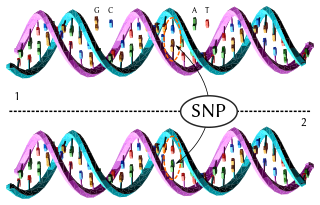
In genetics and bioinformatics, a single-nucleotide polymorphism is a germline substitution of a single nucleotide at a specific position in the genome that is present in a sufficiently large fraction of considered population.

Preimplantation genetic diagnosis is the genetic profiling of embryos prior to implantation, and sometimes even of oocytes prior to fertilization. PGD is considered in a similar fashion to prenatal diagnosis. When used to screen for a specific genetic disease, its main advantage is that it avoids selective abortion, as the method makes it highly likely that the baby will be free of the disease under consideration. PGD thus is an adjunct to assisted reproductive technology, and requires in vitro fertilization (IVF) to obtain oocytes or embryos for evaluation. Embryos are generally obtained through blastomere or blastocyst biopsy. The latter technique has proved to be less deleterious for the embryo, therefore it is advisable to perform the biopsy around day 5 or 6 of development.
A haplotype is a group of alleles in an organism that are inherited together from a single parent.
The International HapMap Project was an organization that aimed to develop a haplotype map (HapMap) of the human genome, to describe the common patterns of human genetic variation. HapMap is used to find genetic variants affecting health, disease and responses to drugs and environmental factors. The information produced by the project is made freely available for research.
Genetics, a discipline of biology, is the science of heredity and variation in living organisms.

A designer baby is a baby whose genetic makeup has been selected or altered, often to exclude a particular gene or to remove genes associated with disease. This process usually involves analysing a wide range of human embryos to identify genes associated with particular diseases and characteristics, and selecting embryos that have the desired genetic makeup; a process known as preimplantation genetic diagnosis. Screening for single genes is commonly practiced, and polygenic screening is offered by a few companies. Other methods by which a baby's genetic information can be altered involve directly editing the genome before birth, which is not routinely performed and only one instance of this is known to have occurred as of 2019, where Chinese twins Lulu and Nana were edited as embryos, causing widespread criticism.

Loss of heterozygosity (LOH) is a type of genetic abnormality in diploid organisms in which one copy of an entire gene and its surrounding chromosomal region are lost. Since diploid cells have two copies of their genes, one from each parent, a single copy of the lost gene still remains when this happens, but any heterozygosity is no longer present.
A genetic marker is a gene or DNA sequence with a known location on a chromosome that can be used to identify individuals or species. It can be described as a variation that can be observed. A genetic marker may be a short DNA sequence, such as a sequence surrounding a single base-pair change, or a long one, like minisatellites.
Genetic association is when one or more genotypes within a population co-occur with a phenotypic trait more often than would be expected by chance occurrence.
A tag SNP is a representative single nucleotide polymorphism (SNP) in a region of the genome with high linkage disequilibrium that represents a group of SNPs called a haplotype. It is possible to identify genetic variation and association to phenotypes without genotyping every SNP in a chromosomal region. This reduces the expense and time of mapping genome areas associated with disease, since it eliminates the need to study every individual SNP. Tag SNPs are useful in whole-genome SNP association studies in which hundreds of thousands of SNPs across the entire genome are genotyped.
Virtual karyotype is the digital information reflecting a karyotype, resulting from the analysis of short sequences of DNA from specific loci all over the genome, which are isolated and enumerated. It detects genomic copy number variations at a higher resolution for level than conventional karyotyping or chromosome-based comparative genomic hybridization (CGH). The main methods used for creating virtual karyotypes are array-comparative genomic hybridization and SNP arrays.
Skewed X-chromosome inactivation occurs when the X-inactivation of one X chromosome is favored over the other, leading to an uneven number of cells with each chromosome inactivated. It is usually defined as one allele being found on the active X chromosome in over 75% of cells, and extreme skewing is when over 90% of cells have inactivated the same X chromosome. It can be caused by primary nonrandom inactivation, either by chance due to a small cell pool or directed by genes, or by secondary nonrandom inactivation, which occurs by selection.
Microfluidic whole genome haplotyping is a technique for the physical separation of individual chromosomes from a metaphase cell followed by direct resolution of the haplotype for each allele.
Disease gene identification is a process by which scientists identify the mutant genotypes responsible for an inherited genetic disorder. Mutations in these genes can include single nucleotide substitutions, single nucleotide additions/deletions, deletion of the entire gene, and other genetic abnormalities.
For preventing Tay–Sachs disease, three main approaches have been used to prevent or reduce the incidence of Tay–Sachs disease in those who are at high risk:
Embryo quality is the ability of an embryo to perform successfully in terms of conferring a high pregnancy rate and/or resulting in a healthy person. Embryo profiling is the estimation of embryo quality by qualification and/or quantification of various parameters. Estimations of embryo quality guides the choice in embryo selection in in vitro fertilization.
Polar body biopsy is the sampling of a polar body of an oocyte. It was first applied clinically in humans in 1987 after extensive animal studies. A polar body is a small haploid cell that is formed concomitantly as an egg cell during oogenesis, but which generally does not have the ability to be fertilized.
References
- 1 2 "Developing a Haplotype Map of the Human Genome to Find Genes Related to Health and Disease: Meeting Summary". www.genome.gov. Retrieved 2016-03-29.
- 1 2 3 Coskun S, Qubbaj W. 2010. Preimplantation genetic diagnosis and selection. J. Reprod Stem Cell Biotechnol 1(1): 120-140.
- ↑ Shamash J, Rienstein S, Wolf-Reznik H, Pras E, Dekel M, Litmanovitch T, Brengauz M, Goldman B, Yonath H, Dor J, Levron J, Aviram-Goldring A. Preimplantation genetic haplotyping a new application for diagnosis of translocation carrier’s embryos- preliminary observations of two robertsonian translocation carrier families. J Assist Reprod Genet (2011) 28:77–83.
- 1 2 Altarescu G, Zeevi DA, Zeligson S, Perlberg S, Eldar-Geva T, Margalioth EJ, Levy-Lahad E, Renbaum P. Familial haplotyping and embryo analysis for Preimplantation Genetic Diagnosis (PGD) microarrays: a proof of principle study. J Assist Reprod Genet (2013) 30:1595–1603.
- ↑ NewsRx. 2015. Genetics; Studies from Sanger Institute in the Area of Human Genetics Reported (Concurrent Whole-Genome Haplotyping and Copy-Number Profiling of Single Cells). Atlanta (GA): Life Science Weekly.
- 1 2 3 Renwick PJ, Trussler J, Ostad-Saffari E, et al. (2006-07-13). "Proof of principle and first cases using preimplantation genetic haplotyping--a paradigm shift for embryo diagnosis". Reprod Biomed Online. 13 (1): 110–9. doi: 10.1016/S1472-6483(10)62024-X . PMID 16820122.
- ↑ Shamash, J. et al. (2011). Preimplantation genetic haplotyping a new application for diagnosis of translocation carrier’s embryos – preliminary observations of two robertsonian trans-location carrier families. Journal of Assisted Reproduction and Genetics, 28(1), 77-83.