Related Research Articles

Medical psychology, or Medico-psychology, is the application of psychological principles to the practice of medicine, primarily drug-oriented, for both physical and mental disorders.
Psychiatric nursing or mental health nursing is the appointed position of a nurse that specialises in mental health, and cares for people of all ages experiencing mental illnesses or distress. These include: neurodevelopmental disorders, schizophrenia, schizoaffective disorder, mood disorders, addiction, anxiety disorders, personality disorders, eating disorders, suicidal thoughts, psychosis, paranoia, and self-harm.
Nursing assessment is the gathering of information about a patient's physiological, psychological, sociological, and spiritual status by a licensed Registered Nurse. Nursing assessment is the first step in the nursing process. A section of the nursing assessment may be delegated to certified nurses aides. Vitals and EKG's may be delegated to certified nurses aides or nursing techs. It differs from a medical diagnosis. In some instances, the nursing assessment is very broad in scope and in other cases it may focus on one body system or mental health. Nursing assessment is used to identify current and future patient care needs. It incorporates the recognition of normal versus abnormal body physiology. Prompt recognition of pertinent changes along with the skill of critical thinking allows the nurse to identify and prioritize appropriate interventions. An assessment format may already be in place to be used at specific facilities and in specific circumstances.

A nurse practitioner (NP) is an advanced practice registered nurse and a type of mid-level practitioner. NPs are trained to assess patient needs, order and interpret diagnostic and laboratory tests, diagnose disease, formulate and prescribe medications and treatment plans. NP training covers basic disease prevention, coordination of care, and health promotion, but does not provide the depth of expertise needed to recognize more complex conditions.

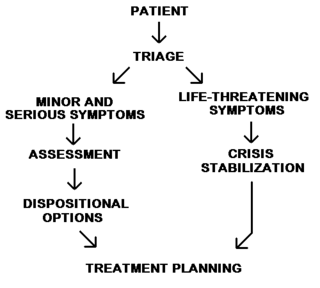
Emergency psychiatry is the clinical application of psychiatry in emergency settings. Conditions requiring psychiatric interventions may include attempted suicide, substance abuse, depression, psychosis, violence or other rapid changes in behavior. Psychiatric emergency services are rendered by professionals in the fields of medicine, nursing, psychology and social work. The demand for emergency psychiatric services has rapidly increased throughout the world since the 1960s, especially in urban areas. Care for patients in situations involving emergency psychiatry is complex.
District Nurses work manage care within the community and lead teams of community nurses and support workers. The role requires registered nurses to take a NMC approved specialist practitioner course. Duties generally include visiting house-bound patients and providing advice and care such as palliative care, wound management, catheter and continence care and medication support. Their work involves both follow-up care for recently discharged hospital inpatients and longer term care for chronically ill patients who may be referred by many other services, as well as working collaboratively with general practitioners in preventing unnecessary or avoidable hospital admissions.
A clinical nurse specialist (CNS) is an advanced practice nurse who can provide advice related to specific conditions or treatment pathways. According to the International Council of Nurses (ICN), an Advanced Practice Nurse is a registered nurse who has acquired the expert knowledge base, complex decision-making skills and clinical competencies for expanded practice, the characteristics of which are shaped by the context and/or country in which s/he is credentialed to practice. Clinical Nurse Specialists are registered nurses, who have graduate level nursing preparation at the master's or doctoral level as a CNS. They are clinical experts in evidence-based nursing practice within a specialty area, treating and managing the health concerns of patients and populations. The CNS specialty may be focused on individuals, populations, settings, type of care, type of problem, or diagnostic systems subspecialty. CNSs practice autonomously and integrate knowledge of disease and medical treatments into the assessment, diagnosis, and treatment of patients' illnesses. These nurses design, implement, and evaluate both patient–specific and population-based programs of care. CNSs provide leadership in the advanced practice of nursing to achieve quality and cost-effective patient outcomes as well as provide leadership of multidisciplinary groups in designing and implementing innovative alternative solutions that address system problems and/or patient care issues. In many jurisdictions, CNSs, as direct care providers, perform comprehensive health assessments, develop differential diagnoses, and may have prescriptive authority. Prescriptive authority allows them to provide pharmacologic and nonpharmacologic treatments and order diagnostic and laboratory tests in addressing and managing specialty health problems of patients and populations. CNSs serve as patient advocates, consultants, and researchers in various settings [American Nurses Association (ANA) Scope and Standards of Practice (2004), p. 15].
Psychiatric and mental health nurses in the U.S. Army Nurse Corps employing groundbreaking protocols and treatments in psychiatric issues to address the unique challenges that our service men and women face, more commonly post-traumatic stress disorder and traumatic brain injuries. Most people understand that trauma exposure is a popular occupational hazard for military members. Psychiatric screenings, before and during their enlistment, and treatments after being exposed to warfare, death, destruction, and torture have been extremely beneficial for military personnel and their dependents.
A mental health professional is a health care practitioner or social and human services provider who offers services for the purpose of improving an individual's mental health or to treat mental disorders. This broad category was developed as a name for community personnel who worked in the new community mental health agencies begun in the 1970s to assist individuals moving from state hospitals, to prevent admissions, and to provide support in homes, jobs, education, and community. These individuals were the forefront brigade to develop the community programs, which today may be referred to by names such as supported housing, psychiatric rehabilitation, supported or transitional employment, sheltered workshops, supported education, daily living skills, affirmative industries, dual diagnosis treatment, individual and family psychoeducation, adult day care, foster care, family services and mental health counseling.

Emergency nursing is a specialty within the field of professional nursing focusing on the care of patients who require prompt medical attention to avoid long-term disability or death. In addition to addressing "true emergencies," emergency nurses increasingly care for people who are unwilling or unable to get primary medical care elsewhere and come to emergency departments for help. In fact, only a small percentage of emergency department (ED) patients have emergency conditions such as a stroke, heart attack or major trauma. Emergency nurses also tend to patients with acute alcohol and/or drug intoxication, psychiatric and behavioral problems and those who have been raped.
In the United States, a psychiatric-mental health nurse practitioner (PMHNP) is an advanced practice registered nurse trained to provide a wide range of mental health services to patients and families in a variety of settings. PMHNPs diagnose, conduct therapy, and prescribe medications for patients who have psychiatric disorders, medical organic brain disorders or substance abuse problems. They are licensed to provide emergency psychiatric services, psychosocial and physical assessment of their patients, treatment plans, and manage patient care. They may also serve as consultants or as educators for families and staff. The PMHNP has a focus on psychiatric diagnosis, including the differential diagnosis of medical disorders with psychiatric symptoms, and on medication treatment for psychiatric disorders.
Chronic care management, encompasses the oversight and education activities conducted by health care professionals to help patients with chronic diseases and health conditions such as diabetes, high blood pressure, systemic lupus erythematosus, multiple sclerosis, and sleep apnea learn to understand their condition and live successfully with it. This term is equivalent to disease management for chronic conditions. The work involves motivating patients to persist in necessary therapies and interventions and helping them to achieve an ongoing, reasonable quality of life.
A psychiatric assessment, or psychological screening, is the process of gathering information about a person within a psychiatric service, with the purpose of making a diagnosis. The assessment is usually the first stage of a treatment process, but psychiatric assessments may also be used for various legal purposes. The assessment includes social and biographical information, direct observations, and data from specific psychological tests. It is typically carried out by a psychiatrist, but it can be a multi-disciplinary process involving nurses, psychologists, occupational therapist, social workers, and licensed professional counselors.

Nursing is a profession within the health care sector focused on the care of individuals, families, and communities so they may attain, maintain, or recover optimal health and quality of life. They also take on vital roles of education, assessing situations, as support. Nurses may be differentiated from other health care providers by their approach to patient care, training, and scope of practice. Nurses practice in many specialties with differing levels of prescription authority. Nurses comprise the largest component of most healthcare environments; but there is evidence of international shortages of qualified nurses. Many nurses provide care within the ordering scope of physicians, and this traditional role has shaped the public image of nurses as care providers. Nurse practitioners are nurses with a graduate degree in advanced practice nursing. They are however permitted by most jurisdictions to practice independently in a variety of settings. Since the postwar period, nurse education has undergone a process of diversification towards advanced and specialized credentials, and many of the traditional regulations and provider roles are changing.
Psychiatry is the medical specialty devoted to the diagnosis, prevention, and treatment of mental disorders. These include various maladaptations related to mood, behaviour, cognition, and perceptions. See glossary of psychiatry.
Kevin Joseph Michael Gournay CBE FMedSci FRCN FRSM FRCPsych (Hon) PhD RN CSci Cert CBT is a registered psychologist, chartered scientist and a registered nurse by background. He is an emeritus professor at the Institute of Psychiatry, King's College London. He was a consultant psychologist at the Priory Hospital North London; retiring in December 2018. He has now returned to clinical work as part of the response to COVID19. He is currently an Honorary Professor at the Matilda Centre; University of Sydney., where his work focusses on the combination of mental health problems and substance use. He has been responsible over many years for a very wide range of research, policy and practice development in mental health care. He also works as an Expert Witness; he has provided reports on more than 300 suicides; 20 homicides and hundreds of reports on people who have suffered the consequences of traumatic events, including accidents, terrorist related incidents, natural disasters, war related events and stillbirth and perinatal death. He has also provided numerous reports on patients receiving care and treatment in high secure and Medium secure settings, including Broadmoor, Rampton and Ashworth hospitals
Unlicensed assistive personnel (UAP) are paraprofessionals who assist individuals with physical disabilities, mental impairments, and other health care needs with their activities of daily living (ADLs). UAPs also provide bedside care—including basic nursing procedures—all under the supervision of a registered nurse, licensed practical nurse or other health care professional. UAPs must demonstrate their ability and competence before gaining any expanded responsibilities in a clinical setting. While providing this care, UAPs offer compassion and patience and are part of the patient's healthcare support system. Communication between UAPs and registered nurses (RNs) is key as they are working together in their patients' best interests. The scope of care UAPs are responsible for is delegated by RNs or other clinical licensed professionals.
A Mental Health Nurse (MHN) refers to a psychiatric nurse in the UK, who specialises in the care of patients with mental health issues.

Correctional nursing or forensic nursing is nursing as it relates to prisoners. Nurses are required in prisons, jails and detention centers; their job is to provide physical and mental healthcare for detainees and inmates. In these correctional settings, nurses are the primary healthcare providers. These nurses also work with victims and assist in expert witness testimonies and are involved in a variety of legal cases including paternity disputes and workplace injuries.
Travel health nursing is a nursing specialty which promotes the health and safety of national and international travelers. Similar to travel medicine, it is an interdisciplinary practice which draws from the knowledge bases of vaccines, epidemiology, tropical medicine, public health, and health education. Travel nursing has experienced an increase in global demand due to the evolution of travel medicine. Travel health nursing was recognized during the 1980s as an emerging occupation to meet the needs of the traveling public, and additional education and training was established. Travel health nurses typically work in "private practice, hospital outpatient units, universities, the government, and the military", and have more opportunities and leadership roles as travel has become more common. However, they also experience organizational and support-related conflicts with general practitioners and patients in healthcare settings.
References
- 1 2 "How to Become a Psychiatric Nurse". All Nursing Schools. Retrieved 2020-06-17.
- 1 2 3 4 Vrklevski, Lila P.; Eljiz, Kathy; Greenfield, David (2017). "The Evolution and Devolution of Mental Health Services in Australia". Inquiries Journal. 9 (10).
- 1 2 3 4 Bazley, Margaret (1973-05-01). "Psychiatric nursing in New Zealand". International Journal of Nursing Studies. 10 (2): 103–110. doi:10.1016/0020-7489(73)90012-6. ISSN 0020-7489. PMID 4488101.
- ↑ Bazley, Margaret (1973-05-01). "Psychiatric nursing in New Zealand". International Journal of Nursing Studies. 10 (2): 104. doi:10.1016/0020-7489(73)90012-6. ISSN 0020-7489. PMID 4488101.
- ↑ Bazley, Margaret (1973-05-01). "Psychiatric nursing in New Zealand". International Journal of Nursing Studies. 10 (2): 106. doi:10.1016/0020-7489(73)90012-6. ISSN 0020-7489. PMID 4488101.
- 1 2 3 "A Brief History of Mental Illness and the U.S. Mental Health Care System". www.uniteforsight.org. Retrieved 2020-06-17.
- 1 2 Nikkonen, Merja (1994). "Caring from the point of view of a Finnish mental health nurse: a life history approach". Journal of Advanced Nursing. 19 (6): 1185–1186. doi:10.1111/j.1365-2648.1994.tb01203.x. ISSN 1365-2648. PMID 7930100.
- ↑ Walsh, Oonagh (2015-07-01). Psychiatric nurses and their patients in the nineteenth century: The Irish perspective. Manchester University Press. p. 28. doi:10.7765/9781784992156.00008. ISBN 978-1-78499-215-6.
- 1 2 3 4 5 Walsh, Oonagh (2015-07-01). Psychiatric nurses and their patients in the nineteenth century: The Irish perspective. Manchester University Press. p. 29. doi:10.7765/9781784992156.00008. ISBN 978-1-78499-215-6.
- ↑ Walsh, Oonagh (2015-07-01). Psychiatric nurses and their patients in the nineteenth century: The Irish perspective. Manchester University Press. p. 47. doi:10.7765/9781784992156.00008. ISBN 978-1-78499-215-6.
- 1 2 Erickson, Isabel (April 1935). "The Psychiatric Nurse". The American Journal of Nursing. 35 (4): 352. doi:10.2307/3411547. JSTOR 3411547.
- 1 2 "Role of Psychiatric Nursing". Work - Chron.com. Retrieved 2020-06-17.
- ↑ Morrissey & Callaghan, Jean & Patrick (2011). Communication skills for mental health nurses. New York, United States of America: McGraw-HIll Education. p. 6.
- ↑ Jones, Adrian (2009). Nurse Prescribing in Mental Health. Hoboken, NJ: Wiley-Blackmore. p. 125.
- 1 2 Jones, Adrian (2009). Nurse prescribing in mental health. Hoboken, NJ: Wiley-Blackmore. p. 126.
- ↑ Jones, Adrian (2009). Nurse Prescribing in Mental Health. Hoboken, NJ: Wiley-Blackmore. p. 127.
- 1 2 Jones, Adrian (2009). Nurse Prescribing in Mental Health. Hoboken, NJ: Wiley-Blackmore. p. 89.
- 1 2 3 4 Jones, Adrian (2009). Nurse Prescribing in Mental Health. Hoboken, NJ: Wiley-Blackmore. p. 91.
- 1 2 Jones, Adrian (2009). Nurse Prescribing in Mental Health. Hoboken, NJ: Wiley-Blackmore. p. 90.
- 1 2 Jones, Adrian (2009). Nurse Prescribing in Mental Health. Hoboken, NJ: Wiley-Blackmore. p. 93.
- 1 2 Jones, Adrian (2009). Nurse Prescribing in Mental Health. Hoboken, NJ: Wiley-Blackmore. p. 94.
- 1 2 Jones, Adrian (2009). Nurse Prescribing in Mental Health. Hoboken, NJ: Wiley-Blackmore. p. 95.
- 1 2 Jones, Adrian (2009). Nurse Prescribing in Mental Health. Hoboken, NJ: Wiley-Blackmore. p. 96.
- ↑ "Becoming a Registered Nurse in Australia | How It's Done & Why It Matters". IHNA Blog. 2016-07-29. Retrieved 2020-06-17.
- 1 2 "Postgraduate Certificate in Health Sciences in Mental Health Nursing at University of Auckland | New Zealand Education | Study in New Zealand". www.studyinnewzealand.govt.nz. Retrieved 2020-06-17.
- 1 2 Hanrahan, Nancy P.; Delaney, Kathleen R.; Stuart, Gail W. (March 2012). "Blueprint for development of the advanced practice psychiatric nurse workforce". Nursing Outlook. 60 (2): 91–104. doi:10.1016/j.outlook.2011.04.007. PMID 21703649.
- 1 2 "Become a Psychiatric Nurse: Here's the Path to Take". blog.jobmedic.co.uk. Retrieved 2020-06-17.
- 1 2 Nelson Mandela University. "Nelson Mandela University Psychiatric Nursing".