Related Research Articles

Hypoxia is a condition in which the body or a region of the body is deprived of adequate oxygen supply at the tissue level. Hypoxia may be classified as either generalized, affecting the whole body, or local, affecting a region of the body. Although hypoxia is often a pathological condition, variations in arterial oxygen concentrations can be part of the normal physiology, for example, during strenuous physical exercise.

Tracheal intubation, usually simply referred to as intubation, is the placement of a flexible plastic tube into the trachea (windpipe) to maintain an open airway or to serve as a conduit through which to administer certain drugs. It is frequently performed in critically injured, ill, or anesthetized patients to facilitate ventilation of the lungs, including mechanical ventilation, and to prevent the possibility of asphyxiation or airway obstruction.

Mechanical ventilation or assisted ventilation is the medical term for using a ventilator machine to fully or partially provide artificial ventilation. Mechanical ventilation helps move air into and out of the lungs, with the main goal of helping the delivery of oxygen and removal of carbon dioxide. Mechanical ventilation is used for many reasons, including to protect the airway due to mechanical or neurologic cause, to ensure adequate oxygenation, or to remove excess carbon dioxide from the lungs. Various healthcare providers are involved with the use of mechanical ventilation and people who require ventilators are typically monitored in an intensive care unit.

In first aid, the recovery position is one of a series of variations on a lateral recumbent or three-quarters prone position of the body, often used for unconscious but breathing casualties.

Intensive care medicine, also called critical care medicine, is a medical specialty that deals with seriously or critically ill patients who have, are at risk of, or are recovering from conditions that may be life-threatening. It includes providing life support, invasive monitoring techniques, resuscitation, and end-of-life care. Doctors in this specialty are often called intensive care physicians, critical care physicians, or intensivists.

Airway management includes a set of maneuvers and medical procedures performed to prevent and relieve airway obstruction. This ensures an open pathway for gas exchange between a patient's lungs and the atmosphere. This is accomplished by either clearing a previously obstructed airway; or by preventing airway obstruction in cases such as anaphylaxis, the obtunded patient, or medical sedation. Airway obstruction can be caused by the tongue, foreign objects, the tissues of the airway itself, and bodily fluids such as blood and gastric contents (aspiration).

Pulse oximetry is a noninvasive method for monitoring blood oxygen saturation. Peripheral oxygen saturation (SpO2) readings are typically within 2% accuracy of the more accurate reading of arterial oxygen saturation (SaO2) from arterial blood gas analysis.

Epiglottitis is the inflammation of the epiglottis—the flap at the base of the tongue that prevents food entering the trachea (windpipe). Symptoms are usually rapid in onset and include trouble swallowing which can result in drooling, changes to the voice, fever, and an increased breathing rate. As the epiglottis is in the upper airway, swelling can interfere with breathing. People may lean forward in an effort to open the airway. As the condition worsens, stridor and bluish skin may occur.
In anaesthesia and advanced airway management, rapid sequence induction (RSI) – also referred to as rapid sequence intubation or as rapid sequence induction and intubation (RSII) or as crash induction – is a special process for endotracheal intubation that is used where the patient is at a high risk of pulmonary aspiration. It differs from other techniques for inducing general anesthesia in that several extra precautions are taken to minimize the time between giving the induction drugs and securing the tube, during which period the patient's airway is essentially unprotected.
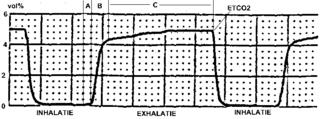
Capnography is the monitoring of the concentration or partial pressure of carbon dioxide (CO
2) in the respiratory gases. Its main development has been as a monitoring tool for use during anesthesia and intensive care. It is usually presented as a graph of CO
2 (measured in kilopascals, "kPa" or millimeters of mercury, "mmHg") plotted against time, or, less commonly, but more usefully, expired volume (known as volumetric capnography). The plot may also show the inspired CO
2, which is of interest when rebreathing systems are being used. When the measurement is taken at the end of a breath (exhaling), it is called "end tidal" CO
2 (PETCO2).

Non-invasive ventilation (NIV) is the use of breathing support administered through a face mask, nasal mask, or a helmet. Air, usually with added oxygen, is given through the mask under positive pressure; generally the amount of pressure is alternated depending on whether someone is breathing in or out. It is termed "non-invasive" because it is delivered with a mask that is tightly fitted to the face or around the head, but without a need for tracheal intubation. While there are similarities with regard to the interface, NIV is not the same as continuous positive airway pressure (CPAP), which applies a single level of positive airway pressure throughout the whole respiratory cycle; CPAP does not deliver ventilation but is occasionally used in conditions also treated with NIV.

Ludwig's angina is a type of severe cellulitis involving the floor of the mouth and is often caused by bacterial sources. Early in the infection, the floor of the mouth raises due to swelling, leading to difficulty swallowing saliva. As a result, patients may present with drooling and difficulty speaking. As the condition worsens, the airway may be compromised and hardening of the spaces on both sides of the tongue may develop. Overall, this condition has a rapid onset over a few hours.

ABC and its variations are initialism mnemonics for essential steps used by both medical professionals and lay persons when dealing with a patient. In its original form it stands for Airway, Breathing, and Circulation. The protocol was originally developed as a memory aid for rescuers performing cardiopulmonary resuscitation, and the most widely known use of the initialism is in the care of the unconscious or unresponsive patient, although it is also used as a reminder of the priorities for assessment and treatment of patients in many acute medical and trauma situations, from first-aid to hospital medical treatment. Airway, breathing, and circulation are all vital for life, and each is required, in that order, for the next to be effective: a viable Airway is necessary for Breathing to provide oxygenated blood for Circulation. Since its development, the mnemonic has been extended and modified to fit the different areas in which it is used, with different versions changing the meaning of letters or adding other letters.
Michael Frass is an Austrian medicine specialist for internal medicine and professor at the Medical University of Vienna (MUW). He is known for his work on homeopathy.

Advanced airway management is the subset of airway management that involves advanced training, skill, and invasiveness. It encompasses various techniques performed to create an open or patent airway – a clear path between a patient's lungs and the outside world.
An aerosol-generating procedure (AGP) is a medical or health-care procedure that a public health agency such as the World Health Organization or the United States Centers for Disease Control and Prevention (CDC) has designated as creating an increased risk of transmission of an aerosol borne contagious disease, such as COVID-19. The presumption is that the risk of transmission of the contagious disease from a patient having an AGP performed on them is higher than for a patient who is not having an AGP performed upon them. This then informs decisions on infection control, such as what personal protective equipment (PPE) is required by a healthcare worker performing the medical procedure, or what PPE healthcare workers are allowed to use.

Proning or prone positioning is the placement of patients into a prone position so that they are lying on their front. This is used in the treatment of patients in intensive care with acute respiratory distress syndrome (ARDS). It has been especially tried and studied for patients on ventilators but, during the COVID-19 pandemic, it is being used for patients with oxygen masks and CPAP as an alternative to ventilation.

Suction Assisted Laryngoscopy Airway Decontamination (SALAD) is incremental step-wise approach to the management of a massively contaminated airway.

Silent hypoxia is generalised hypoxia that does not coincide with shortness of breath. This presentation is known to be a complication of COVID-19, and is also known in walking pneumonia, altitude sickness, and rebreather diving.
Calvin Johnson is an American anesthesiologist and professor of anesthesiology at Cedars-Sinai Medical Center in Los Angeles, California. Born and raised in Egelston Township, Muskegon, Michigan, Johnson attended Oakridge High School, where he excelled in multiple sports and was a first-team Associated Press all-state basketball player. He went on to play point guard at Dartmouth College, earning Academic All-American honors and ranked second for assists in the Ivy League during his senior year.
References
- 1 2 3 Dwyer, Jim (April 3, 2020). "The Doctor Came to Save Lives. The Co-op Board Told Him to Get Lost". The New York Times. Retrieved April 24, 2020.
- 1 2 "Diane Edbril and Richard Levitan Are Married". New York Times. January 8, 1990. Retrieved May 8, 2020.
- 1 2 "About Airway Cam". Airway Cam. Retrieved May 2, 2020.
- 1 2 "Richard M. Levitan MD - Littleton Regional Healthcare". littletonhealthcare.org. Retrieved April 25, 2020.
- 1 2 3 4 Levitan, Richard (April 20, 2020). "Opinion | The Infection That's Silently Killing Coronavirus Patients". The New York Times. ISSN 0362-4331 . Retrieved April 24, 2020.
- ↑ Koziol, John (April 15, 2020). "Littleton doctor returns from NYC with COVID-19 insights". Union Leader. Retrieved April 25, 2020.
- ↑ "Richard M Levitan, MD – Faculty Expertise Database – Geisel School of Medicine at Dartmouth" . Retrieved April 26, 2020.
- 1 2 April 23, CBS News. "Device that checks oxygen levels could be early warning system for coronavirus, doctor says". www.cbsnews.com. Retrieved April 24, 2020.
{{cite news}}: CS1 maint: numeric names: authors list (link) - ↑ Carbone, Christopher (April 23, 2020). "'Silent hypoxia' may be killing COVID-19 patients, but one doctor offers a possible solution". Fox News. Retrieved April 24, 2020.
- ↑ Couzin-Frankel, Jennifer (April 28, 2020). "Why don't some coronavirus patients sense their alarmingly low oxygen levels?". Science. American Association for the Advancement of Science (AAAS). doi:10.1126/science.abc5107. ISSN 0036-8075. S2CID 219024882.
- ↑ Shah, Sonia; Majmudar, Kaushal; Stein, Amy; Gupta, Nita; Suppes, Spencer; Karamanis, Marina; Capannari, Joseph; Sethi, Sanjay; Patte, Christine (July 23, 2020). Kline, Jeffrey A. (ed.). "Novel Use of Home Pulse Oximetry Monitoring in COVID-19 Patients Discharged From the Emergency Department Identifies Need for Hospitalization". Academic Emergency Medicine. 27 (8). Wiley: 681–692. doi:10.1111/acem.14053. ISSN 1069-6563. PMC 7323027 . PMID 32779828.
- ↑ Levitan, Richard M. (2020). Kline, Jeffrey A. (ed.). "Pulse Oximetry as a Biomarker for Early Identification and Hospitalization of COVID-19 Pneumonia". Academic Emergency Medicine. 27 (8). Wiley: 785–786. doi: 10.1111/acem.14052 . ISSN 1069-6563. PMC 7323007 . PMID 32779867. S2CID 220251166.
- ↑ Reviews of the Airway Cam Guide to Intubation and Practical Emergency Airway Management
- Ovassapian, Andranik (September 2005). "The Airway Cam Guide to Intubation and Practical Emergency Airway Management (review)". Anesthesia & Analgesia. 101 (3): 930. doi: 10.1097/00000539-200509000-00078 .
- Doyle, D. John (2005). "The Airway Cam™ guide to intubation and practical emergency airway management (review)". Canadian Journal of Anesthesia. 52 (4). Springer Science and Business Media LLC: 448. doi: 10.1007/bf03016302 . ISSN 0832-610X.
- Rocchini, Albert J. (2006). "The Airway Cam Guide to Intubation and Practical Emergency Airway Management (review)". Prehospital Emergency Care. 10 (2). Informa UK Limited: 276–277. doi:10.1080/10903120500540995. ISSN 1090-3127. S2CID 71173379.
- ↑ Hayes, Alisa (2016). "2015 EMRA/AIRWAY CAM: Fundamentals of Airway Management, 3rd Edition (review)". Annals of Emergency Medicine. 67 (5). Elsevier BV: 685. doi: 10.1016/j.annemergmed.2016.02.029 . ISSN 0196-0644.