Tracheal intubation, usually simply referred to as intubation, is the placement of a flexible plastic tube into the trachea (windpipe) to maintain an open airway or to serve as a conduit through which to administer certain drugs. It is frequently performed in critically injured, ill, or anesthetized patients to facilitate ventilation of the lungs, including mechanical ventilation, and to prevent the possibility of asphyxiation or airway obstruction.

Mechanical ventilation or assisted ventilation is the medical term for using a machine called a ventilator to fully or partially provide artificial ventilation. Mechanical ventilation helps move air into and out of the lungs, with the main goal of helping the delivery of oxygen and removal of carbon dioxide. Mechanical ventilation is used for many reasons, including to protect the airway due to mechanical or neurologic cause, to ensure adequate oxygenation, or to remove excess carbon dioxide from the lungs. Various healthcare providers are involved with the use of mechanical ventilation and people who require ventilators are typically monitored in an intensive care unit.

Laryngoscopy is endoscopy of the larynx, a part of the throat. It is a medical procedure that is used to obtain a view, for example, of the vocal folds and the glottis. Laryngoscopy may be performed to facilitate tracheal intubation during general anaesthesia or cardiopulmonary resuscitation or for surgical procedures on the larynx or other parts of the upper tracheobronchial tree.

Airway management includes a set of maneuvers and medical procedures performed to prevent and relieve airway obstruction. This ensures an open pathway for gas exchange between a patient's lungs and the atmosphere. This is accomplished by either clearing a previously obstructed airway; or by preventing airway obstruction in cases such as anaphylaxis, the obtunded patient, or medical sedation. Airway obstruction can be caused by the tongue, foreign objects, the tissues of the airway itself, and bodily fluids such as blood and gastric contents (aspiration).

Respiratory arrest is a serious medical condition caused by apnea or respiratory dysfunction severe enough that it will not sustain the body. Prolonged apnea refers to a patient who has stopped breathing for a long period of time. If the heart muscle contraction is intact, the condition is known as respiratory arrest. An abrupt stop of pulmonary gas exchange lasting for more than five minutes may permanently damage vital organs, especially the brain. Lack of oxygen to the brain causes loss of consciousness. Brain injury is likely if respiratory arrest goes untreated for more than three minutes, and death is almost certain if more than five minutes.

Epiglottitis is the inflammation of the epiglottis—the flap at the base of the tongue that prevents food entering the trachea (windpipe). Symptoms are usually rapid in onset and include trouble swallowing which can result in drooling, changes to the voice, fever, and an increased breathing rate. As the epiglottis is in the upper airway, swelling can interfere with breathing. People may lean forward in an effort to open the airway. As the condition worsens, stridor and bluish skin may occur.
In anaesthesia and advanced airway management, rapid sequence induction (RSI) – also referred to as rapid sequence intubation or as rapid sequence induction and intubation (RSII) or as crash induction – is a special process for endotracheal intubation that is used where the patient is at a high risk of pulmonary aspiration. It differs from other techniques for inducing general anesthesia in that several extra precautions are taken to minimize the time between giving the induction drugs and securing the tube, during which period the patient's airway is essentially unprotected.

Ludwig's angina is a type of severe cellulitis involving the floor of the mouth and is often caused by bacterial sources. Early in the infection, the floor of the mouth raises due to swelling, leading to difficulty swallowing saliva. As a result, patients may present with drooling and difficulty speaking. As the condition worsens, the airway may be compromised and hardening of the spaces on both sides of the tongue may develop. Overall, this condition has a rapid onset over a few hours.

A cricothyrotomy is an incision made through the skin and cricothyroid membrane to establish a patent airway during certain life-threatening situations, such as airway obstruction by a foreign body, angioedema, or massive facial trauma. Cricothyrotomy is nearly always performed as a last resort in cases where other means of tracheal intubation are impossible or impractical. Compared with tracheotomy, cricothyrotomy is quicker and easier to perform, does not require manipulation of the cervical spine, and is associated with fewer complications. However, while cricothyrotomy may be life-saving in extreme circumstances, this technique is only intended to be a temporizing measure until a definitive airway can be established.

In anesthesia, the Mallampati score or Mallampati classification, named after the Indian anaesthesiologist Seshagiri Mallampati, is used to predict the ease of endotracheal intubation. The test comprises a visual assessment of the distance from the tongue base to the roof of the mouth, and therefore the amount of space in which there is to work. It is an indirect way of assessing how difficult an intubation will be; this is more definitively scored using the Cormack–Lehane classification system, which describes what is actually seen using direct laryngoscopy during the intubation process itself. A high Mallampati score is associated with more difficult intubation as well as a higher incidence of sleep apnea.
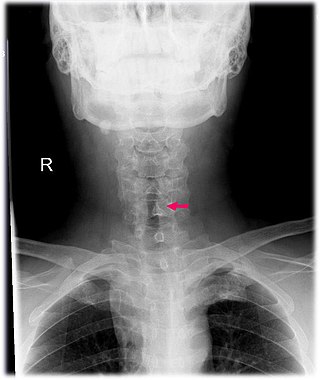
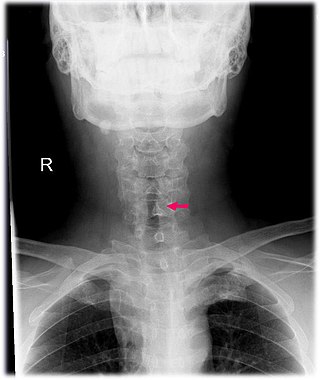
Subglottic stenosis is a congenital or acquired narrowing of the subglottic airway. It can be congenital, acquired, iatrogenic, or very rarely, idiopathic. It is defined as the narrowing of the portion of the airway that lies between the vocal cords and the lower part of the cricoid cartilage. In a normal infant, the subglottic airway is 4.5-5.5 millimeters wide, while in a premature infant, the normal width is 3.5 millimeters. Subglottic stenosis is defined as a diameter of under 4 millimeters in an infant. Acquired cases are more common than congenital cases due to prolonged intubation being introduced in the 1960s. It is most frequently caused by certain medical procedures or external trauma, although infections and systemic diseases can also cause it.

Bronchoscopy is an endoscopic technique of visualizing the inside of the airways for diagnostic and therapeutic purposes. An instrument (bronchoscope) is inserted into the airways, usually through the nose or mouth, or occasionally through a tracheostomy. This allows the practitioner to examine the patient's airways for abnormalities such as foreign bodies, bleeding, tumors, or inflammation. Specimens may be taken from inside the lungs. The construction of bronchoscopes ranges from rigid metal tubes with attached lighting devices to flexible optical fiber instruments with realtime video equipment.
Mouth infections, also known as oral infections, are a group of infections that occur around the oral cavity. They include dental infection, dental abscess, and Ludwig's angina. Mouth infections typically originate from dental caries at the root of molars and premolars that spread to adjacent structures. In otherwise healthy patients, removing the offending tooth to allow drainage will usually resolve the infection. In cases that spread to adjacent structures or in immunocompromised patients, surgical drainage and systemic antibiotics may be required in addition to tooth extraction. Since bacteria that normally reside in the oral cavity cause mouth infections, proper dental hygiene can prevent most cases of infection. As such, mouth infections are more common in populations with poor access to dental care or populations with health-related behaviors that damage one's teeth and oral mucosa. This is a common problem, representing nearly 36% of all encounters within the emergency department related to dental conditions.

Tracheobronchial injury is damage to the tracheobronchial tree. It can result from blunt or penetrating trauma to the neck or chest, inhalation of harmful fumes or smoke, or aspiration of liquids or objects.
Procedural sedation and analgesia (PSA) is a technique in which a sedating/dissociative medication is given, usually along with an analgesic medication, in order to perform non-surgical procedures on a patient. The overall goal is to induce a decreased level of consciousness while maintaining the patient's ability to breathe on their own. Airway protective reflexes are not compromised by this process and therefore endotracheal intubation is not required. PSA is commonly used in the emergency department, in addition to the operating room.
A sari is a female garment in the Indian subcontinent.
The Cormack–Lehane system classifies views obtained by direct laryngoscopy based on the structures seen. It was initially described by R.S. Cormack and J. Lehane in 1984 as a way of simulating potential scenarios that trainee anaesthetists might face. A modified version that subdivided Grade 2 was initially described in 1998.

Airtraq is a fibreoptic intubation device used for indirect tracheal intubation in difficult airway situations. It is designed to enable a view of the glottic opening without aligning the oral with the pharyngeal, and laryngeal axes as an advantage over direct endotracheal intubation and allows for intubation with minimal head manipulation and positioning.
Thyromental distance (TMD) measurement is a method commonly used to predict the difficulty of intubation and is measured from the thyroid notch to the tip of the jaw with the head extended. If it is less than 7.0 cm with hard scarred tissues, it indicates possible difficult intubation.

Advanced airway management is the subset of airway management that involves advanced training, skill, and invasiveness. It encompasses various techniques performed to create an open or patent airway – a clear path between a patient's lungs and the outside world.