Related Research Articles
Intensive insulin therapy or flexible insulin therapy is a therapeutic regimen for diabetes mellitus treatment. This newer approach contrasts with conventional insulin therapy. Rather than minimize the number of insulin injections per day, the intensive approach favors flexible meal times with variable carbohydrate as well as flexible physical activities. The trade-off is the increase from 2 or 3 injections per day to 4 or more injections per day, which was considered "intensive" relative to the older approach. In North America in 2004, many endocrinologists prefer the term "flexible insulin therapy" (FIT) to "intensive therapy" and use it to refer to any method of replacing insulin that attempts to mimic the pattern of small continuous basal insulin secretion of a working pancreas combined with larger insulin secretions at mealtimes. The semantic distinction reflects changing treatment.
Insulin resistance (IR) is a pathological condition in which cells in insulin-sensitive tissues in the body fail to respond normally to the hormone insulin or downregulate insulin receptors in response to hyperinsulinemia.

The glucose tolerance test is a medical test in which glucose is given and blood samples taken afterward to determine how quickly it is cleared from the blood. The test is usually used to test for diabetes, insulin resistance, impaired beta cell function, and sometimes reactive hypoglycemia and acromegaly, or rarer disorders of carbohydrate metabolism. In the most commonly performed version of the test, an oral glucose tolerance test (OGTT), a standard dose of glucose is ingested by mouth and blood levels are checked two hours later. Many variations of the GTT have been devised over the years for various purposes, with different standard doses of glucose, different routes of administration, different intervals and durations of sampling, and various substances measured in addition to blood glucose.

Hyperglycemia or hyperglycaemia is a condition in which an excessive amount of glucose (glucotoxicity) circulates in the blood plasma. This is generally a blood sugar level higher than 11.1 mmol/L (200 mg/dL), but symptoms may not start to become noticeable until even higher values such as 13.9–16.7 mmol/L (~250–300 mg/dL). A subject with a consistent fasting blood glucose range between ~5.6 and ~7 mmol/L is considered slightly hyperglycemic, and above 7 mmol/L is generally held to have diabetes. For diabetics, glucose levels that are considered to be too hyperglycemic can vary from person to person, mainly due to the person's renal threshold of glucose and overall glucose tolerance. On average, however, chronic levels above 10–12 mmol/L (180–216 mg/dL) can produce noticeable organ damage over time.

Type 2 diabetes (T2D), formerly known as adult-onset diabetes, is a form of diabetes mellitus that is characterized by high blood sugar, insulin resistance, and relative lack of insulin. Common symptoms include increased thirst, frequent urination, fatigue and unexplained weight loss. Other symptoms include increased hunger, having a sensation of pins and needles, and sores (wounds) that heal slowly. Symptoms often develop slowly. Long-term complications from high blood sugar include heart disease, stroke, diabetic retinopathy, which can result in blindness, kidney failure, and poor blood flow in the lower-limbs, which may lead to amputations. The sudden onset of hyperosmolar hyperglycemic state may occur; however, ketoacidosis is uncommon.

The blood sugar level, blood sugar concentration, blood glucose level, or glycemia is the measure of glucose concentrated in the blood. The body tightly regulates blood glucose levels as a part of metabolic homeostasis.

Prednisone is a glucocorticoid medication mostly used to suppress the immune system and decrease inflammation in conditions such as asthma, COPD, and rheumatologic diseases. It is also used to treat high blood calcium due to cancer and adrenal insufficiency along with other steroids. It is taken by mouth.

Gestational diabetes is a condition in which a woman without diabetes develops high blood sugar levels during pregnancy. Gestational diabetes generally results in few symptoms; however, it increases the risk of pre-eclampsia, depression, and of needing a Caesarean section. Babies born to individuals with poorly treated gestational diabetes are at increased risk of macrosomia, of having hypoglycemia after birth, and of jaundice. If untreated, diabetes can also result in stillbirth. Long term, children are at higher risk of being overweight and of developing type 2 diabetes.
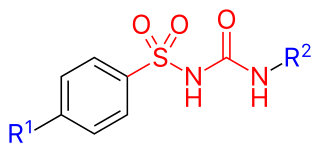
Sulfonylureas or sulphonylureas are a class of organic compounds used in medicine and agriculture. The functional group consists of a sulfonyl group (-S(=O)2) with its sulphur atom bonded to a nitrogen atom of a ureylene group (N,N-dehydrourea, a dehydrogenated derivative of urea). The side chains R1 and R2 distinguish various sulfonylureas. Sulfonylureas are the most widely used herbicide.
Maturity-onset diabetes of the young (MODY) refers to any of several hereditary forms of diabetes mellitus caused by mutations in an autosomal dominant gene disrupting insulin production. Along with neonatal diabetes, MODY is a form of the conditions known as monogenic diabetes. While the more common types of diabetes involve more complex combinations of causes involving multiple genes and environmental factors, each forms of MODY are caused by changes to a single gene (monogenic). HNF1A-MODY are the most common forms.
Glycated hemoglobin is a form of hemoglobin (Hb) that is chemically linked to a sugar.
Stress hyperglycemia is a medical term referring to transient elevation of the blood glucose due to the stress of illness. It usually resolves spontaneously, but must be distinguished from various forms of diabetes mellitus.

Type 1 diabetes (T1D), formerly known as juvenile diabetes, is an autoimmune disease that occurs when pancreatic are destroyed by the body's immune system. Insulin is a hormone required by the body to store and convert blood sugar into energy. T1D results in high blood sugar levels in the body prior to treatment. Common symptoms include frequent urination, increased thirst, increased hunger, weight loss, and other complications. Additional symptoms may include blurry vision, tiredness, and slow wound healing. While some cases take longer, symptoms usually appear within weeks or a few months.
The main goal of diabetes management is to keep blood glucose levels as normal as possible. If diabetes is not well controlled, further challenges to health may occur. People with diabetes can measure blood sugar by various methods, such as with a blood glucose meter or a continuous glucose monitor, which monitors over several days. Glucose can also be measured by analysis of a routine blood sample. Usually, people are recommended to control diet, exercise, and maintain a healthy weight, although some people may need medications to control their blood sugar levels. Other goals of diabetes management are to prevent or treat complications that can result from the disease itself and from its treatment.
Alpha-glucosidase inhibitors (AGIs) are oral anti-diabetic drugs used for diabetes mellitus type 2 that work by preventing the digestion of carbohydrates. Carbohydrates are normally converted into simple sugars (monosaccharides) by alpha-glucosidase enzymes present on cells lining the intestine, enabling monosaccharides to be absorbed through the intestine. Hence, alpha-glucosidase inhibitors reduce the impact of dietary carbohydrates on blood sugar.

Prediabetes is a component of metabolic syndrome and is characterized by elevated blood sugar levels that fall below the threshold to diagnose diabetes mellitus. It usually does not cause symptoms but people with prediabetes often have obesity, dyslipidemia with high triglycerides and/or low HDL cholesterol, and hypertension. It is also associated with increased risk for cardiovascular disease (CVD). Prediabetes is more accurately considered an early stage of diabetes as health complications associated with type 2 diabetes often occur before the diagnosis of diabetes.
The dawn phenomenon, sometimes called the dawn effect, is an observed increase in blood sugar (glucose) levels that takes place in the early-morning, often between 2 a.m. and 8 a.m. First described by Schmidt in 1981 as an increase of blood glucose or insulin demand occurring at dawn, this naturally occurring phenomenon is frequently seen among the general population and is clinically relevant for patients with diabetes as it can affect their medical management. In contrast to Chronic Somogyi rebound, the dawn phenomenon is not associated with nocturnal hypoglycemia.

As a medication, insulin is any pharmaceutical preparation of the protein hormone insulin that is used to treat high blood glucose. Such conditions include type 1 diabetes, type 2 diabetes, gestational diabetes, and complications of diabetes such as diabetic ketoacidosis and hyperosmolar hyperglycemic states. Insulin is also used along with glucose to treat hyperkalemia. Typically it is given by injection under the skin, but some forms may also be used by injection into a vein or muscle. There are various types of insulin, suitable for various time spans. The types are often all called insulin in the broad sense, although in a more precise sense, insulin is identical to the naturally occurring molecule whereas insulin analogues have slightly different molecules that allow for modified time of action. It is on the World Health Organization's List of Essential Medicines. In 2021, it was the 179th most commonly prescribed medication in the United States, with more than 2 million prescriptions.
Complications of diabetes are secondary diseases that are a result of elevated blood glucose levels that occur in diabetic patients. These complications can be divided into two types: acute and chronic. Acute complications are complications that develop rapidly and can be exemplified as diabetic ketoacidosis (DKA), hyperglycemic hyperosmolar state (HHS), lactic acidosis (LA), and hypoglycemia. Chronic complications develop over time and are generally classified in two categories: microvascular and macrovascular. Microvascular complications include neuropathy, nephropathy, and retinopathy; while cardiovascular disease, stroke, and peripheral vascular disease are included in the macrovascular complications.

Diabetes mellitus, often known simply as diabetes, is a group of common endocrine diseases characterized by sustained high blood sugar levels. Diabetes is due to either the pancreas not producing enough insulin, or the cells of the body becoming unresponsive to the hormone's effects. Classic symptoms include thirst, polyuria, weight loss, and blurred vision. If left untreated, the disease can lead to various health complications, including disorders of the cardiovascular system, eye, kidney, and nerves. Diabetes accounts for approximately 4.2 million deaths every year, with an estimated 1.5 million caused by either untreated or poorly treated diabetes.
References
- 1 2 3 4 5 Hwang, Jessica L.; Weiss, Roy E. (2014). "Steroid-induced diabetes: a clinical and molecular approach to understanding and treatment". Diabetes/Metabolism Research and Reviews. 30 (2). Wiley: 96–102. doi:10.1002/dmrr.2486. ISSN 1520-7552. PMC 4112077 . PMID 24123849.
- 1 2 Kim, Seo Yun; Yoo, Chul-Gyu; Lee, Chun Taeg; Chung, Hee Soon; Kim, Young Whan; Han, Sung Koo; Shim, Young-Soo; Yim, Jae-Joon (2011). "Incidence and Risk Factors of Steroid-induced Diabetes in Patients with Respiratory Disease". Journal of Korean Medical Science. 26 (2). Korean Academy of Medical Sciences: 264–267. doi:10.3346/jkms.2011.26.2.264. ISSN 1011-8934. PMC 3031012 . PMID 21286019.
- ↑ Ha, YJ; Lee, K-H; Jung, SJ; Lee, S-W; Lee, S-K; Park, Y-B (June 9, 2011). "Glucocorticoid-induced diabetes mellitus in patients with systemic lupus erythematosus treated with high-dose glucocorticoid therapy". Lupus. 20 (10). SAGE Publications: 1027–1034. doi:10.1177/0961203311402246. ISSN 0961-2033. PMID 21659423. S2CID 6767818.
- ↑ MAZZANTINI, MAURIZIO; TORRE, CLAUDIA; MICCOLI, MARIO; BAGGIANI, ANGELO; TALARICO, ROSARIA; BOMBARDIERI, STEFANO; DI MUNNO, OMBRETTA (January 15, 2012). "Adverse Events During Longterm Low-dose Glucocorticoid Treatment of Polymyalgia Rheumatica: A Retrospective Study". The Journal of Rheumatology. 39 (3): 552–557. doi:10.3899/jrheum.110851. ISSN 0315-162X. PMID 22247343.
- ↑ Van Laecke, S.; Van Biesen, W.; Verbeke, F.; De Bacquer, D.; Peeters, P.; Vanholder, R. (2009). "Posttransplantation Hypomagnesemia and Its Relation with Immunosuppression as Predictors of New-Onset Diabetes after Transplantation". American Journal of Transplantation. 9 (9). Elsevier BV: 2140–2149. doi: 10.1111/j.1600-6143.2009.02752.x . ISSN 1600-6135. PMID 19624560.
- ↑ Baid, Seema; Cosimi, A. Benedict; Lin Farrell, Mary; Schoenfeld, David A.; Feng, Sandy; Chung, Raymond T.; Tolkoff-Rubin, Nina; Pascual, Manuel (2001). "Posttransplant Diabetes Mellitus in Liver Transplant Recipients: Risk Factors, Temporal Relationship with Hepatitis C Virus Allograft Hepatitis, and Impact on Mortality1". Transplantation. 72 (6). Ovid Technologies (Wolters Kluwer Health): 1066–1072. doi:10.1097/00007890-200109270-00015. ISSN 0041-1337. PMID 11579302.
- ↑ Bahtiyar, Gül; Shin, John J.; Aytaman, Ayse; Sowers, James R.; McFarlane, Samy I. (2004). "Association of diabetes and hepatitis C infection: Epidemiologic evidence and pathophysiologic insights". Current Diabetes Reports. 4 (3). Springer Science and Business Media LLC: 194–198. doi:10.1007/s11892-004-0023-7. ISSN 1534-4827. PMID 15132884. S2CID 45679334.
- ↑ "Diagnosis and Classification of Diabetes Mellitus". Diabetes Care. 35 (Supplement_1). American Diabetes Association: S64–S71. December 13, 2011. doi:10.2337/dc12-s064. ISSN 0149-5992. PMC 3632174 . PMID 22187472.