Related Research Articles

Antipsychotics, previously known as neuroleptics and major tranquilizers, are a class of psychotropic medication primarily used to manage psychosis, principally in schizophrenia but also in a range of other psychotic disorders. They are also the mainstay, together with mood stabilizers, in the treatment of bipolar disorder. Moreover, they are also used as adjuncts in the treatment of treatment-resistant major depressive disorder.

Clozapine, sold under the brand name Clozaril among others, is a psychiatric medication and was the first atypical antipsychotic to be discovered. It is primarily used to treat people with schizophrenia and schizoaffective disorder who have had an inadequate response to two other antipsychotics, or who have been unable to tolerate other drugs due to extrapyramidal side effects. In the US the FDA authorisation also includes use for people with recurrent suicidal behaviour in people with schizophrenia or schizoaffective disorder. It is also used for the treatment of psychosis in Parkinson's disease.

Neuroleptic malignant syndrome (NMS) is a rare but life-threatening reaction that can occur in response to antipsychotics (neuroleptic) or other drugs that block the effects of dopamine. Symptoms include high fever, confusion, rigid muscles, variable blood pressure, sweating, and fast heart rate. Complications may include muscle breakdown (rhabdomyolysis), high blood potassium, kidney failure, or seizures.

Haloperidol, sold under the brand name Haldol among others, is a typical antipsychotic medication. Haloperidol is used in the treatment of schizophrenia, tics in Tourette syndrome, mania in bipolar disorder, delirium, agitation, acute psychosis, and hallucinations from alcohol withdrawal. It may be used by mouth or injection into a muscle or a vein. Haloperidol typically works within 30 to 60 minutes. A long-acting formulation may be used as an injection every four weeks for people with schizophrenia or related illnesses, who either forget or refuse to take the medication by mouth.

Fluphenazine, sold under the brand name Prolixin among others, is a high-potency typical antipsychotic medication. It is used in the treatment of chronic psychoses such as schizophrenia, and appears to be about equal in effectiveness to low-potency antipsychotics like chlorpromazine. It is given by mouth, injection into a muscle, or just under the skin. There is also a long acting injectable version that may last for up to four weeks. Fluphenazine decanoate, the depot injection form of fluphenazine, should not be used by people with severe depression.

Typical antipsychotics are a class of antipsychotic drugs first developed in the 1950s and used to treat psychosis. Typical antipsychotics may also be used for the treatment of acute mania, agitation, and other conditions. The first typical antipsychotics to come into medical use were the phenothiazines, namely chlorpromazine which was discovered serendipitously. Another prominent grouping of antipsychotics are the butyrophenones, an example of which is haloperidol. The newer, second-generation antipsychotics, also known as atypical antipsychotics, have largely supplanted the use of typical antipsychotics as first-line agents due to the higher risk of movement disorders with typical antipsychotics.

The atypical antipsychotics (AAP), also known as second generation antipsychotics (SGAs) and serotonin–dopamine antagonists (SDAs), are a group of antipsychotic drugs largely introduced after the 1970s and used to treat psychiatric conditions. Some atypical antipsychotics have received regulatory approval for schizophrenia, bipolar disorder, irritability in autism, and as an adjunct in major depressive disorder.

Quetiapine, sold under the brand name Seroquel among others, is an atypical antipsychotic medication used for the treatment of schizophrenia, bipolar disorder, and major depressive disorder. Despite being widely used as a sleep aid, the benefits of such use may not outweigh the risk of undesirable side effects. It is taken orally.

Perphenazine is a typical antipsychotic drug. Chemically, it is classified as a piperazinyl phenothiazine. Originally marketed in the United States as Trilafon, it has been in clinical use for decades.
Tardive dyskinesia (TD) is an iatrogenic disorder that results in involuntary repetitive body movements, which may include grimacing, sticking out the tongue or smacking the lips, which occurs following treatment with medication. Additional motor symptoms include chorea or athetosis. In about 20% of people with TD, the disorder interferes with daily functioning. If TD is present in the setting of a long-term drug therapy, reversibility can be determined primarily by severity of symptoms and how long symptoms have been present before the long-term drug has been stopped.
The dopamine hypothesis of schizophrenia or the dopamine hypothesis of psychosis is a model that attributes the positive symptoms of schizophrenia to a disturbed and hyperactive dopaminergic signal transduction. The model draws evidence from the observation that a large number of antipsychotics have dopamine-receptor antagonistic effects. The theory, however, does not posit dopamine overabundance as a complete explanation for schizophrenia. Rather, the overactivation of D2 receptors, specifically, is one effect of the global chemical synaptic dysregulation observed in this disorder.

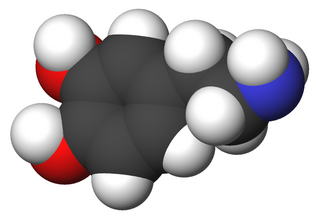
A dopamine antagonist, also known as an anti-dopaminergic and a dopamine receptor antagonist (DRA), is a type of drug which blocks dopamine receptors by receptor antagonism. Most antipsychotics are dopamine antagonists, and as such they have found use in treating schizophrenia, bipolar disorder, and stimulant psychosis. Several other dopamine antagonists are antiemetics used in the treatment of nausea and vomiting.

Amisulpride, sold under the brand names Solian and Barhemsys, is a medication used in the treatment of schizophrenia, acute psychotic episodes, depression, and nausea and vomiting. It is specifically used at lower doses intravenously to prevent and treat postoperative nausea and vomiting; at low doses by mouth to treat depression; and at higher doses by mouth to treat psychosis.
Extrapyramidal symptoms (EPS) are symptoms that are archetypically associated with the extrapyramidal system of the brain's cerebral cortex. When such symptoms are caused by medications or other drugs, they are also known as extrapyramidal side effects (EPSE). The symptoms can be acute (short-term) or chronic (long-term). They include movement dysfunction such as dystonia, akathisia, parkinsonism characteristic symptoms such as rigidity, bradykinesia, tremor, and tardive dyskinesia. Extrapyramidal symptoms are a reason why subjects drop out of clinical trials of antipsychotics; of the 213 (14.6%) subjects that dropped out of one of the largest clinical trials of antipsychotics, 58 (27.2%) of those discontinuations were due to EPS.

Melperone is an atypical antipsychotic of the butyrophenone chemical class, making it structurally related to the typical antipsychotic haloperidol. It first entered clinical use in 1960s.
NMDA receptor modulators are a new form of antipsychotic that are in Phase II FDA studies. The first compound studied was glycine which was hypothesized by Daniel Javitt after observation that people with phencyclidine(PCP)-induced psychosis were lacking in glutamate transmission. In giving glycine to people with PCP-induced psychosis a recovery rate was noted. From there, it was hypothesized that people with psychosis from schizophrenia would benefit from increased glutamate transmission and glycine was added with strong recovery rates noted especially in the area of negative and cognitive symptoms. Glycine, however, sporadic results aside remains an adjunct antipsychotic and an unworkable compound. However, the Eli Lilly and Company study drug LY-2140023 is being studied as a primary antipsychotic and is showing strong recovery rates, especially in the area of negative and cognitive symptoms of schizophrenia. Tardive dyskinesia, diabetes and other standard complications have not been noted:
Treatment with LY2140023, like treatment with olanzapine, was safe and well-tolerated; treated patients showed statistically significant improvements in both positive and negative symptoms of schizophrenia compared to placebo. Notably, patients treated with LY-2140023 did not differ from placebo-treated patients with respect to prolactin elevation, extrapyramidal symptoms or weight gain. These data suggest that mGlu2/3 receptor agonists have antipsychotic properties and may provide a new alternative for the treatment of schizophrenia.

Aripiprazole lauroxil, sold under the brand name Aristada, is a long-acting injectable atypical antipsychotic that was developed by Alkermes. It is an N-acyloxymethyl prodrug of aripiprazole that is administered via intramuscular injection once every four to eight weeks for the treatment of schizophrenia. Aripiprazole lauroxil was approved by the U.S. Food and Drug Administration (FDA) on 5 October 2015.
Dopamine supersensitivity psychosis is a hypothesis that attempts to explain the phenomenon in which psychosis (e.g., hallucinations, delusions) occurs despite treatment with escalating doses of antipsychotics. Dopamine supersensitivity may be caused by the dopamine receptor D2 antagonizing effect of antipsychotics, causing a compensatory increase in D2 receptors within the brain that sensitizes neurons to endogenous release of the neurotransmitter dopamine. Because psychosis is thought to be mediated—at least in part—by the activity of dopamine at D2 receptors, the activity of dopamine in the presence of supersensitivity may paradoxically give rise to worsening psychotic symptoms despite antipsychotic treatment at a given dose. This phenomenon may co-occur with tardive dyskinesia, a rare movement disorder that may also be due to dopamine supersensitivity.

Antipsychotic switching refers to the process of switching out one antipsychotic for another antipsychotic. There are multiple indications for switching antipsychotics, including inadequate efficacy and drug intolerance. There are several strategies that have been theorized for antipsychotic switching, based upon the timing of discontinuation and tapering of the original antipsychotic and the timing of initiation and titration of the new antipsychotic. Major adverse effects from antipsychotic switching may include supersensitivity syndromes, withdrawal, and rebound syndromes.
References
- ↑ McCarthy, John J. (1978). "Tardive Psychosis". American Journal of Psychiatry. 135 (5): 625–626. doi:10.1176/ajp.135.5.625-b. ISSN 0002-953X.
- 1 2 Palmstierna, T; Wistedt, B (1988). "Tardive psychosis: Does it exist?". Psychopharmacology. 94 (1): 144–5. doi:10.1007/BF00735897. PMID 2894699.
- ↑ Chouinard, G; Jones, BD (1980). "Neuroleptic-induced supersensitivity psychosis: Clinical and pharmacological characteristics". Am J Psychiatry. 137 (1): 16–21. doi:10.1176/ajp.137.1.16. PMID 6101522.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Swartz, Conrad M. (2004-10-01). "Antipsychotic Psychosis". Psychiatric Times. 21 (12): 17.
- ↑ Wilson, I. C; Garbutt, J. C; Lanier, C. F; Moylan, J; Nelson, W; Prange, A. J (1983). "Is There a Tardive Dysmentia?". Schizophrenia Bulletin. 9 (2): 187–92. doi: 10.1093/schbul/9.2.187 . PMID 6135252.
- ↑ Ross, David E (2004). "Clozapine and Typical Antipsychotics". American Journal of Psychiatry. 161 (10): 1925–6. doi:10.1176/ajp.161.10.1925-a. PMID 15465996.