An advance healthcare directive, also known as living will, personal directive, advance directive, medical directive or advance decision, is a legal document in which a person specifies what actions should be taken for their health if they are no longer able to make decisions for themselves because of illness or incapacity. In the U.S. it has a legal status in itself, whereas in some countries it is legally persuasive without being a legal document.
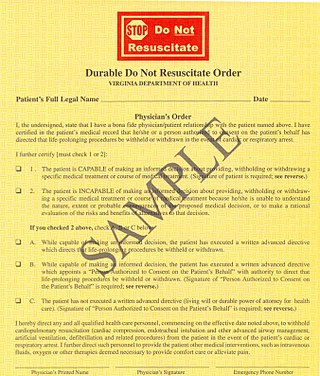
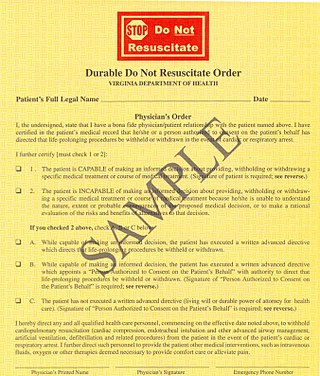
A do-not-resuscitate order (DNR), also known as Do Not Attempt Resuscitation (DNAR), Do Not Attempt Cardiopulmonary Resuscitation (DNACPR), no code or allow natural death, is a medical order, written or oral depending on the jurisdiction, indicating that a person should not receive cardiopulmonary resuscitation (CPR) if that person's heart stops beating. Sometimes these decisions and the relevant documents also encompass decisions around other critical or life-prolonging medical interventions. The legal status and processes surrounding DNR orders vary in different polities. Most commonly, the order is placed by a physician based on a combination of medical judgement and patient involvement.
Medical ethics is an applied branch of ethics which analyzes the practice of clinical medicine and related scientific research. Medical ethics is based on a set of values that professionals can refer to in the case of any confusion or conflict. These values include the respect for autonomy, non-maleficence, beneficence, and justice. Such tenets may allow doctors, care providers, and families to create a treatment plan and work towards the same common goal. These four values are not ranked in order of importance or relevance and they all encompass values pertaining to medical ethics. However, a conflict may arise leading to the need for hierarchy in an ethical system, such that some moral elements overrule others with the purpose of applying the best moral judgement to a difficult medical situation. Medical ethics is particularly relevant in decisions regarding involuntary treatment and involuntary commitment.
The right to die is a concept based on the opinion that human beings are entitled to end their life or undergo voluntary euthanasia. Possession of the right to die is often bestowed with the understanding that a person with a terminal illness, incurable pain, or without the will to continue living should be allowed to end their own life, use assisted suicide, or decline life-prolonging treatment. The question of who, if anyone, may be empowered to make this decision is often the subject of debate.
Measure 16 of 1994 established the U.S. state of Oregon's Death with Dignity Act, which legalizes medical aid in dying with certain restrictions. Passage of this initiative made Oregon the first U.S. state and one of the first jurisdictions in the world to permit some terminally ill patients to determine the time of their own death.

Primary care is a model of care that supports first-contact, accessible, continuous, comprehensive and coordinated person-focused care. It aims to optimise population health and reduce disparities across the population by ensuring that subgroups have equal access to services.
Terminal illness or end-stage disease is a disease that cannot be cured or adequately treated and is expected to result in the death of the patient. This term is more commonly used for progressive diseases such as cancer, dementia or advanced heart disease than for injury. In popular use, it indicates a disease that will progress until death with near absolute certainty, regardless of treatment. A patient who has such an illness may be referred to as a terminal patient, terminally ill or simply as being terminal. There is no standardized life expectancy for a patient to be considered terminal, although it is generally months or less. Life expectancy for terminal patients is a rough estimate given by the physician based on previous data and does not always reflect true longevity. An illness which is lifelong but not fatal is a chronic condition.
Futile medical care is the continued provision of medical care or treatment to a patient when there is no reasonable hope of a cure or benefit.

The terms medical record, health record and medical chart are used somewhat interchangeably to describe the systematic documentation of a single patient's medical history and care across time within one particular health care provider's jurisdiction. A medical record includes a variety of types of "notes" entered over time by healthcare professionals, recording observations and administration of drugs and therapies, orders for the administration of drugs and therapies, test results, X-rays, reports, etc. The maintenance of complete and accurate medical records is a requirement of health care providers and is generally enforced as a licensing or certification prerequisite.
The case of Sun Hudson concerned Wanda Hudson and her infant son, who was allowed to die via removal of his breathing tube, contrary to her wishes.
Spiro Nikolouzos was a Texas man incapacitated from bleeding related to a cerebral shunt, whose care was the subject of an appeal of The Texas Futile Care Law.
The Patient Self-Determination Act (PSDA) was passed by the United States Congress in 1990 as an amendment to the Omnibus Budget Reconciliation Act of 1990. Effective on December 1, 1991, this legislation required many hospitals, nursing homes, home health agencies, hospice providers, health maintenance organizations (HMOs), and other health care institutions to provide information about advance health care directives to adult patients upon their admission to the healthcare facility. This law does not apply to individual physicians.
Tirhas Habtegiris was a United States resident originally from Eritrea, who, after being diagnosed as terminally ill, was removed from a respirator against the wishes of her family. Habtegiris had a form of cancer known as an abdominal angiosarcoma which had spread to her lungs.
Involuntary euthanasia is currently illegal in all 50 states of the United States. Assisted suicide is legal in 10 jurisdictions in the US: Washington, D.C. and the states of California, Colorado, Oregon, Vermont, New Mexico, Maine, New Jersey, Hawaii, and Washington. The status of assisted suicide is disputed in Montana, though currently authorized per the Montana Supreme Court's ruling in Baxter v. Montana that "nothing in Montana Supreme Court precedent or Montana statutes [indicates] that physician aid in dying is against public policy."
Ambulatory care nursing is the nursing care of patients who receive treatment on an outpatient basis, ie they do not require admission to a hospital for an overnight stay. Ambulatory care includes those clinical, organizational and professional activities engaged in by registered nurses with and for individuals, groups, and populations who seek assistance with improving health and/or seek care for health-related problems. The American Academy of Ambulatory Care Nursing (AAACN) describes ambulatory care nursing as a comprehensive practice which is built on a broad knowledge base of nursing and health sciences, and applies clinical expertise rooted in the nursing process.
The Family Health Care Decisions Act is a New York State statute that enables a patient's family member or close friend to make health care treatment decisions if the patient lacks capacity and did not make the decision in advance or appoint a health care agent. It also creates a bedside process to determine patient incapacity; a priority list for the selection of the decision-maker; and ethical standards for making decisions, including life-sustaining treatment decisions. In short, it empowers a surrogate decision-maker for health care decisions for incapable patients in New York.
A surrogate decision maker, also known as a health care proxy or as agents, is an advocate for incompetent patients. If a patient is unable to make decisions for themselves about personal care, a surrogate agent must make decisions for them. If there is a durable power of attorney for health care, the agent appointed by that document is authorized to make health care decisions within the scope of authority granted by the document. If people have court-appointed guardians with authority to make health care decisions, the guardian is the authorized surrogate.
POLST is an approach to improving end-of-life care in the United States, encouraging providers to speak with the severely ill and create specific medical orders to be honored by health care workers during a medical crisis. POLST began in Oregon in 1991 and currently exists in 46 states, British Columbia, and South Korea. The POLST document is a standardized, portable, brightly colored single page medical order that documents a conversation between a provider and an individual with a serious illness or frailty towards the end of life. A POLST form allows emergency medical services to provide treatment that the individual prefers before possibly transporting to an emergency facility.
Maternal somatic support after brain death occurs when a brain dead patient is pregnant and their body is kept alive to deliver a fetus. It occurs very rarely internationally. Even among brain dead patients, in a U.S. study of 252 brain dead patients from 1990–96, only 5 (2.8%) cases involved pregnant women between 15 and 45 years of age.
Involuntary commitment or civil commitment is a legal process through which an individual who is deemed by a qualified agent to have symptoms of severe mental disorder is detained in a psychiatric hospital (inpatient) where they can be treated involuntarily.