Related Research Articles

Platelets or thrombocytes are a blood component whose function is to react to bleeding from blood vessel injury by clumping, thereby initiating a blood clot. Platelets have no cell nucleus; they are fragments of cytoplasm derived from the megakaryocytes of the bone marrow or lung, which then enter the circulation. Platelets are found only in mammals, whereas in other vertebrates, thrombocytes circulate as intact mononuclear cells.

Coagulation, also known as clotting, is the process by which blood changes from a liquid to a gel, forming a blood clot. It results in hemostasis, the cessation of blood loss from a damaged vessel, followed by repair. The process of coagulation involves activation, adhesion and aggregation of platelets, as well as deposition and maturation of fibrin.

Disseminated intravascular coagulation (DIC) is a condition in which blood clots form throughout the body, blocking small blood vessels. Symptoms may include chest pain, shortness of breath, leg pain, problems speaking, or problems moving parts of the body. As clotting factors and platelets are used up, bleeding may occur. This may include blood in the urine, blood in the stool, or bleeding into the skin. Complications may include organ failure.
Factor V Leiden is a variant of human factor V, which causes an increase in blood clotting (hypercoagulability). Due to this mutation, protein C, an anticoagulant protein that normally inhibits the pro-clotting activity of factor V, is not able to bind normally to factor V, leading to a hypercoagulable state, i.e., an increased tendency for the patient to form abnormal and potentially harmful blood clots. Factor V Leiden is the most common hereditary hypercoagulability disorder amongst ethnic Europeans. It is named after the Dutch city of Leiden, where it was first identified in 1994 by Rogier Maria Bertina under the direction of Pieter Hendrik Reitsma. Despite the increased risk of venous thromboembolisms, people with one copy of this gene have not been found to have shorter lives than the general population. It is an autosomal dominant genetic disorder with incomplete penetrance.

The prothrombin time (PT) – along with its derived measures of prothrombin ratio (PR) and international normalized ratio (INR) – is an assay for evaluating the extrinsic pathway and common pathway of coagulation. This blood test is also called protime INR and PT/INR. They are used to determine the clotting tendency of blood, in such things as the measure of warfarin dosage, liver damage, and vitamin K status. PT measures the following coagulation factors: I (fibrinogen), II (prothrombin), V (proaccelerin), VII (proconvertin), and X.

The partial thromboplastin time (PTT), also known as the activated partial thromboplastin time, is a blood test that characterizes coagulation of the blood. A historical name for this measure is the Kaolin-cephalin clotting time (KCCT), reflecting kaolin and cephalin as materials historically used in the test. Apart from detecting abnormalities in blood clotting, partial thromboplastin time is also used to monitor the treatment effect of heparin, a widely prescribed drug that reduces blood's tendency to clot.
Mixing studies are tests performed on blood plasma of patients or test subjects to distinguish factor deficiencies from factor inhibitors, such as lupus anticoagulant, or specific factor inhibitors, such as antibodies directed against factor VIII. Mixing studies are screening tests widely performed in coagulation laboratories. The basic purpose of these tests is to determine the cause of prolongation of Prothrombin Time (PT), Partial Thromboplastin Time, or sometimes of thrombin time (TT). Mixing studies take advantage of the fact that factor levels that are 50 percent of normal should give a normal Prothrombin time (PT) or Partial thromboplastin time (PTT) result.
Lupus anticoagulant is an immunoglobulin that binds to phospholipids and proteins associated with the cell membrane. Its name is a partial misnomer, as it is actually a prothrombotic antibody in vivo. The name derives from their properties in vitro, as these antibodies increase coagulation times in laboratory tests such as the activated partial thromboplastin time (aPTT). Investigators speculate that the antibodies interfere with phospholipids used to induce in vitro coagulation. In vivo, the antibodies are thought to interact with platelet membrane phospholipids, increasing adhesion and aggregation of platelets, which accounts for the in vivo prothrombotic characteristics.

Coagulation factor X, or Stuart factor, is an enzyme of the coagulation cascade, encoded in humans by F10 gene. It is a serine endopeptidase. Factor X is synthesized in the liver and requires vitamin K for its synthesis.

Dilute Russell's viper venom time (dRVVT) is a laboratory test often used for detection of lupus anticoagulant (LA). It is an assessment of the time for blood to clot in the presence of a diluted amount of venom from Russell's viper, a highly venomous snake native to the Indian subcontinent and named after the herpetologist Patrick Russell.
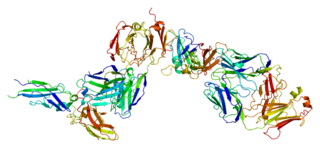
Tissue factor, also called platelet tissue factor or Coagulation factor III, is a protein present in subendothelial tissue and leukocytes which plays a major role in coagulation and, in humans, is encoded by F3 gene. Its role in the blood clotting is the initiation of thrombin formation from the zymogen prothrombin. Thromboplastin defines the cascade that leads to the activation of factor X—the tissue factor pathway. In doing so, it has replaced the previously named extrinsic pathway in order to eliminate ambiguity.
Thromboelastography (TEG) is a method of testing the efficiency of blood coagulation. It is a test mainly used in surgery and anesthesiology, although increasingly used in resuscitations in emergency departments, intensive care units, and labor and delivery suites. More common tests of blood coagulation include prothrombin time (PT) and partial thromboplastin time (aPTT) which measure coagulation factor function, but TEG also can assess platelet function, clot strength, and fibrinolysis which these other tests cannot.

Factor VII deficiency is a bleeding disorder characterized by a lack in the production of Factor VII (FVII) (proconvertin), a protein that causes blood to clot in the coagulation cascade. After a trauma factor VII initiates the process of coagulation in conjunction with tissue factor in the extrinsic pathway.
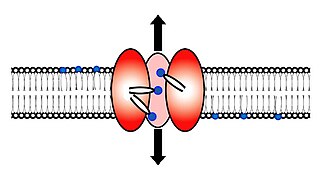
Scramblase is a protein responsible for the translocation of phospholipids between the two monolayers of a lipid bilayer of a cell membrane. In humans, phospholipid scramblases (PLSCRs) constitute a family of five homologous proteins that are named as hPLSCR1–hPLSCR5. Scramblases are members of the general family of transmembrane lipid transporters known as flippases. Scramblases are distinct from flippases and floppases. Scramblases, flippases, and floppases are three different types of enzymatic groups of phospholipid transportation enzymes. The inner-leaflet, facing the inside of the cell, contains negatively charged amino-phospholipids and phosphatidylethanolamine. The outer-leaflet, facing the outside environment, contains phosphatidylcholine and sphingomyelin. Scramblase is an enzyme, present in the cell membrane, that can transport (scramble) the negatively charged phospholipids from the inner-leaflet to the outer-leaflet, and vice versa.

The thrombin time (TT), also known as the thrombin clotting time (TCT), is a blood test that measures the time it takes for a clot to form in the plasma of a blood sample containing anticoagulant, after an excess of thrombin has been added. It is used to diagnose blood coagulation disorders and to assess the effectiveness of fibrinolytic therapy. This test is repeated with pooled plasma from normal patients. The difference in time between the test and the 'normal' indicates an abnormality in the conversion of fibrinogen to fibrin, an insoluble protein.
Clotting time is a general term for the time required for a sample of blood to form a clot, or, in medical terms, coagulate. The term "clotting time" is often used when referring to tests such as the prothrombin time (PT), activated partial thromboplastin time, activated clotting time (ACT), thrombin time (TT), or Reptilase time. These tests are coagulation studies performed to assess the natural clotting ability of a sample of blood. In a clinical setting, healthcare providers will order one of these tests to evaluate a patient's blood for any abnormalities in the time it takes for their blood to clot. Each test involves adding a specific substance to the blood and measuring the time until the blood forms fibrin which is one of the first signs of clotted blood. Each test points to a different component of the clotting sequence which is made up of coagulation factors that help form clots. Abnormal results could be due to a number of reasons including, but, not limited to, deficiency in clotting factors, dysfunction of clotting factors, blood-thinning medications, medication side-effects, platelet deficiency, inherited bleeding or clotting disorders, liver disease, or advanced illness resulting in a medical emergency known as disseminated intravascular coagulation (DIC).
A coagulation screen is a combination of screening laboratory tests, designed to provide rapid non-specific information, which allows an initial broad categorization of haemostatic problems.
The fibrinolysis system is responsible for removing blood clots. Hyperfibrinolysis describes a situation with markedly enhanced fibrinolytic activity, resulting in increased, sometimes catastrophic bleeding. Hyperfibrinolysis can be caused by acquired or congenital reasons. Among the congenital conditions for hyperfibrinolysis, alpha-2-plasmin inhibitor deficiency or plasminogen activator inhibitor type 1 (PAI-1) are very rare. The affected individuals show a hemophilia-like bleeding phenotype. Acquired hyperfibrinolysis is found in liver disease, in patients with severe trauma, during major surgical procedures, and other conditions. A special situation with temporarily enhanced fibrinolysis is thrombolytic therapy with drugs which activate plasminogen, e.g. for use in acute ischemic events or in patients with stroke. In patients with severe trauma, hyperfibrinolysis is associated with poor outcome. Moreover, hyperfibrinolysis may be associated with blood brain barrier impairment, a plasmin-dependent effect due to an increased generation of bradykinin.
Thromboelastometry (TEM), previously named rotational thromboelastography (ROTEG) or rotational thromboelastometry (ROTEM), is an established viscoelastic method for hemostasis testing in whole blood. It is a modification of traditional thromboelastography (TEG).
Blood clotting tests are the tests used for diagnostics of the hemostasis system. Coagulometer is the medical laboratory analyzer used for testing of the hemostasis system. Modern coagulometers realize different methods of activation and observation of development of blood clots in blood or in blood plasma.
References
- ↑ Milstone JH (1964). "Thrombokinase as Prime Activator of Prothrombin: Historical Perspectives and Present Status". Federation Proceedings. 23: 742–748. PMID 14195457.
- ↑ Carlsen E, Stinessen MB, Prydz H (November 1987). "Differential effect of alpha-interferon and gamma-interferon on thromboplastin response in monocytes and endothelial cells". Clinical and Experimental Immunology. 70 (2): 471–8. PMC 1542100 . PMID 3123108.
- ↑ van den Besselaar AM, Chantarangkul V, Tripodi A (July 2010). "Thromboplastin standards". Biologicals. 38 (4): 430–6. doi:10.1016/j.biologicals.2010.02.012. PMID 20338779.