Related Research Articles

Tourette syndrome or Tourette's syndrome is a common neurodevelopmental disorder that begins in childhood or adolescence. It is characterized by multiple movement (motor) tics and at least one vocal (phonic) tic. Common tics are blinking, coughing, throat clearing, sniffing, and facial movements. These are typically preceded by an unwanted urge or sensation in the affected muscles known as a premonitory urge, can sometimes be suppressed temporarily, and characteristically change in location, strength, and frequency. Tourette's is at the more severe end of a spectrum of tic disorders. The tics often go unnoticed by casual observers.

Coprolalia is involuntary swearing or the involuntary utterance of obscene words or socially inappropriate and derogatory remarks. The word comes from the Greek κόπρος, meaning "dung, feces", and λαλιά "speech", from λαλεῖν "to talk".

A tic is a sudden and repetitive motor movement or vocalization that is not rhythmic and involves discrete muscle groups. It is typically brief and may resemble a normal behavioral characteristic or gesture.
Adult Attention Deficit Hyperactivity Disorder is the persistence of attention deficit hyperactivity disorder (ADHD) into adulthood. It is a neurodevelopmental disorder, meaning impairing symptoms must have been present in childhood, except for when ADHD occurs after traumatic brain injury. Specifically, multiple symptoms must be present before the age of 12, according to DSM-5 diagnostic criteria. The cutoff age of 12 is a change from the previous requirement of symptom onset, which was before the age of 7 in the DSM-IV. This was done to add flexibility in the diagnosis of adults. ADHD was previously thought to be a childhood disorder that improved with age, but recent research has disproved this. Approximately two-thirds of childhood cases of ADHD continue into adulthood, with varying degrees of symptom severity that change over time and continue to affect individuals with symptoms ranging from minor inconveniences to impairments in daily functioning.
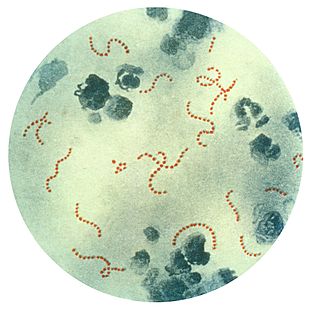
Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS) is a controversial hypothetical diagnosis for a subset of children with rapid onset of obsessive-compulsive disorder (OCD) or tic disorders. Symptoms are proposed to be caused by group A streptococcal (GAS), and more specifically, group A beta-hemolytic streptococcal (GABHS) infections. OCD and tic disorders are hypothesized to arise in a subset of children as a result of a post-streptococcal autoimmune process. The proposed link between infection and these disorders is that an autoimmune reaction to infection produces antibodies that interfere with basal ganglia function, causing symptom exacerbations, and this autoimmune response results in a broad range of neuropsychiatric symptoms.
Stereotypic movement disorder (SMD) is a motor disorder with onset in childhood involving restrictive and/or repetitive, nonfunctional motor behavior, that markedly interferes with normal activities or results in bodily injury. To be classified as SMD, the behavior in question must not be due to the direct effects of a substance, autism, or another medical condition. The cause of this disorder is not known.

An intrusive thought is an unwelcome, involuntary thought, image, or unpleasant idea that may become an obsession, is upsetting or distressing, and can feel difficult to manage or eliminate. When such thoughts are associated with obsessive-compulsive disorder (OCD), Tourette's syndrome (TS), depression, body dysmorphic disorder (BDD), and sometimes attention-deficit hyperactivity disorder (ADHD), the thoughts may become paralyzing, anxiety-provoking, or persistent. Intrusive thoughts may also be associated with episodic memory, unwanted worries or memories from OCD, post-traumatic stress disorder, other anxiety disorders, eating disorders, or psychosis. Intrusive thoughts, urges, and images are of inappropriate things at inappropriate times, and generally have aggressive, sexual, or blasphemous themes.
Societal and cultural aspects of Tourette syndrome include legal advocacy and health insurance issues, awareness of notable individuals with Tourette syndrome, and treatment of TS in the media and popular culture.
Tourette syndrome is an inherited neurodevelopmental disorder that begins in childhood or adolescence, characterized by the presence of motor and phonic tics. The management of Tourette syndrome has the goal of managing symptoms to achieve optimum functioning, rather than eliminating symptoms; not all persons with Tourette's require treatment, and there is no cure or universally effective medication. Explanation and reassurance alone are often sufficient treatment; education is an important part of any treatment plan.
Causes and origins of Tourette syndrome have not been fully elucidated. Tourette syndrome is an inherited neurodevelopmental disorder that begins in childhood or adolescence, characterized by the presence of multiple motor tics and at least one phonic tic, which characteristically wax and wane. Tourette's syndrome occurs along a spectrum of tic disorders, which includes transient tics and chronic tics.
The Yale–Brown Obsessive–Compulsive Scale (Y-BOCS) is a test to rate the severity of obsessive–compulsive disorder (OCD) symptoms.

Tourette syndrome (TS) is an inherited neurological disorder that begins in childhood or adolescence, characterized by the presence of multiple physical (motor) tics and at least one vocal (phonic) tic.

Obsessive–compulsive disorder (OCD) is a mental disorder in which an individual has intrusive thoughts and feels the need to perform certain routines (compulsions) repeatedly to relieve the distress caused by the obsession, to the extent where it impairs general function.
Mental disorders diagnosed in childhood can be neurodevelopmental, emotional, or behavioral disorders. These disorders negatively impact the mental and social wellbeing of a child, and children with these disorders require support from their families and schools. Childhood mental disorders often persist into adulthood. These disorders are usually first diagnosed in infancy, childhood, or adolescence, as laid out in the DSM-5 and in the ICD-11.
The Behavior Rating Inventory of Executive Function (BRIEF) is an assessment of executive function behaviors at home and at school for children and adolescents ages 5–18. It was originally developed by Gerard Gioia, Peter Isquith, Steven Guy, and Lauren Kenworthy
The Yale Global Tic Severity Scale (YGTSS) is a psychological measure designed to assess the severity and frequency of symptoms of disorders such as tic disorder, Tourette syndrome, and obsessive-compulsive disorder, in children and adolescents between ages 6 and 17.
The Child Mania Rating Scales (CMRS) is a 21-item diagnostic screening measure designed to identify symptoms of mania in children and adolescents aged 9–17 using diagnostic criteria from the DSM-IV, developed by Pavuluri and colleagues. There is also a 10-item short form. The measure assesses the child's mood and behavior symptoms, asking parents or teachers to rate how often the symptoms have caused a problem for the youth in the past month. Clinical studies have found the CMRS to be reliable and valid when completed by parents in the assessment of children's bipolar symptoms. The CMRS also can differentiate cases of pediatric bipolar disorder from those with ADHD or no disorder, as well as delineating bipolar subtypes. A meta-analysis comparing the different rating scales available found that the CMRS was one of the best performing scales in terms of telling cases with bipolar disorder apart from other clinical diagnoses. The CMRS has also been found to provide a reliable and valid assessment of symptoms longitudinally over the course of treatment. The combination of showing good reliability and validity across multiple samples and clinical settings, along with being free and brief to score, make the CMRS a promising tool, especially since most other checklists available for youths do not assess manic symptoms.
The Dimensional Obsessive-Compulsive Scale (DOCS) is a 20-item self-report instrument that assesses the severity of Obsessive-Compulsive Disorder (OCD) symptoms along four empirically supported theme-based dimensions: (a) contamination, (b) responsibility for harm and mistakes, (c) incompleteness/symmetry, and (d) unacceptable (taboo) thoughts. The scale was developed in 2010 by a team of experts on OCD led by Jonathan Abramowitz, PhD to improve upon existing OCD measures and advance the assessment and understanding of OCD. The DOCS contains four subscales that have been shown to have good reliability, validity, diagnostic sensitivity, and sensitivity to treatment effects in a variety of settings cross-culturally and in different languages. As such, the DOCS meets the needs of clinicians and researchers who wish to measure current OCD symptoms or assess changes in symptoms over time.
The Child and Adolescent Symptom Inventory (CASI) is a behavioral rating checklist created by Kenneth Gadow and Joyce Sprafkin that evaluates a range of behaviors related to common emotional and behavioral disorders identified in the Diagnostic and Statistical Manual of Mental Disorders (DSM), including attention deficit hyperactivity disorder, oppositional defiant disorder, conduct disorder, generalized anxiety disorder, social phobia, separation anxiety disorder, major depressive episode, mania, dysthymic disorder, schizophrenia, autism spectrum, Asperger syndrome, anorexia, and bulimia. In addition, one or two key symptoms from each of the following disorders are also included: obsessive-compulsive disorder, specific phobia, panic attack, motor/vocal tics, and substance use. CASI combines the Child Symptom Inventory (CSI) and the Adolescent Symptom Inventory (ASI), letting it apply to both children and adolescents, aged from 5 to 18. The CASI is a self-report questionnaire completed by the child's caretaker or teacher to detect signs of psychiatric disorders in multiple settings. Compared to other widely used checklists for youths, the CASI maps more closely to DSM diagnoses, with scoring systems that map to the diagnostic criteria as well as providing a severity score. Other measures are more likely to have used statistical methods, such as factor analysis, to group symptoms that often occur together; if they have DSM-oriented scales, they are often later additions that only include some of the diagnostic criteria.
The Motor tic, Obsessions and compulsions, Vocal tic Evaluation Survey (MOVES) is a psychological measure used to screen for tics and other behaviors. It measures "motor tics, vocal tics, obsessions, compulsions, and associated symptoms including echolalia, echopraxia, coprolalia, and copropraxia".
References
- ↑ Müller N (2007). "Tourette's syndrome: clinical features, pathophysiology, and therapeutic approaches". Dialogues Clin Neurosci (Review). 9 (2): 161–171. doi:10.31887/DCNS.2007.9.2/nmueller. PMC 3181853 . PMID 17726915.
- 1 2 3 4 5 6 7 8 9 10 Shytle RD, Silver AA, Sheehan KH, Wilkinson BJ, Newman M, Sanberg PR, Sheehan D (September 2003). "The Tourette's Disorder Scale (TODS): development, reliability, and validity". Assessment (Clinical trial). 10 (3): 273–287. doi:10.1177/1073191103255497. PMID 14503651.
- 1 2 Szejko N, Robinson S, Hartmann A, et al. (October 2021). "European clinical guidelines for Tourette syndrome and other tic disorders-version 2.0. Part I: assessment". Eur Child Adolesc Psychiatry. 31 (3): 383–402. doi:10.1007/s00787-021-01842-2. PMC 8521086 . PMID 34661764.
- 1 2 3 4 Martino D, Pringsheim TM, Cavanna AE, et al. (March 2017). "Systematic review of severity scales and screening instruments for tics: Critique and recommendations". Mov. Disord. (Review). 32 (3): 467–473. doi:10.1002/mds.26891. PMC 5482361 . PMID 28071825.
- ↑ Sukhodolsky DG, Gladstone TR, Kaushal SA, Piasecka JB, Leckman JF (2017). "Tics and Tourette Syndrome". In Matson JL (ed.). Handbook of Childhood Psychopathology and Developmental Disabilities Treatment. Autism and Child Psychopathology Series. p. 248.
- 1 2 3 4 5 Storch EA, Merlo LJ, Lehmkuhl H, Grabill KM, Geffken GR, Goodman WK, Murphy TK (August 2007). "Further psychometric examination of the Tourette's Disorder Scales". Child Psychiatry Hum Dev (Primary study). 38 (2): 89–98. doi:10.1007/s10578-006-0043-4. PMID 17136450.