Related Research Articles

Pneumonia is an inflammatory condition of the lung primarily affecting the small air sacs known as alveoli. Symptoms typically include some combination of productive or dry cough, chest pain, fever, and difficulty breathing. The severity of the condition is variable.

The trachea, also known as the windpipe, is a cartilaginous tube that connects the larynx to the bronchi of the lungs, allowing the passage of air, and so is present in almost all animals with lungs. The trachea extends from the larynx and branches into the two primary bronchi. At the top of the trachea, the cricoid cartilage attaches it to the larynx. The trachea is formed by a number of horseshoe-shaped rings, joined together vertically by overlying ligaments, and by the trachealis muscle at their ends. The epiglottis closes the opening to the larynx during swallowing.

Sputum is mucus that is coughed up from the lower airways. In medicine, sputum samples are usually used for a naked eye examination, microbiological investigation of respiratory infections and cytological investigations of respiratory systems. It is crucial that the specimen does not include any mucoid material from the nose or oral cavity.

Mechanical ventilation or assisted ventilation is the medical term for using a machine called a ventilator to fully or partially provide artificial ventilation. Mechanical ventilation helps move air into and out of the lungs, with the main goal of helping the delivery of oxygen and removal of carbon dioxide. Mechanical ventilation is used for many reasons, including to protect the airway due to mechanical or neurologic cause, to ensure adequate oxygenation, or to remove excess carbon dioxide from the lungs. Various healthcare providers are involved with the use of mechanical ventilation and people who require ventilators are typically monitored in an intensive care unit.

The respiratory tract is the subdivision of the respiratory system involved with the process of conducting air to the alveoli for the purposes of gas exchange in mammals. The respiratory tract is lined with respiratory epithelium as respiratory mucosa.

A bronchus is a passage or airway in the lower respiratory tract that conducts air into the lungs. The first or primary bronchi to branch from the trachea at the carina are the right main bronchus and the left main bronchus. These are the widest bronchi, and enter the right lung, and the left lung at each hilum. The main bronchi branch into narrower secondary bronchi or lobar bronchi, and these branch into narrower tertiary bronchi or segmental bronchi. Further divisions of the segmental bronchi are known as 4th order, 5th order, and 6th order segmental bronchi, or grouped together as subsegmental bronchi. The bronchi, when too narrow to be supported by cartilage, are known as bronchioles. No gas exchange takes place in the bronchi.

Bronchiectasis is a disease in which there is permanent enlargement of parts of the airways of the lung. Symptoms typically include a chronic cough with mucus production. Other symptoms include shortness of breath, coughing up blood, and chest pain. Wheezing and nail clubbing may also occur. Those with the disease often get lung infections.

Pulmonary aspiration is the entry of material such as pharyngeal secretions, food or drink, or stomach contents from the oropharynx or gastrointestinal tract, into the larynx and lower respiratory tract, the portions of the respiratory system from the trachea (windpipe) to the lungs. A person may inhale the material, or it may be delivered into the tracheobronchial tree during positive pressure ventilation. When pulmonary aspiration occurs during eating and drinking, the aspirated material is often colloquially referred to as "going down the wrong pipe".
Atypical pneumonia, also known as walking pneumonia, is any type of pneumonia not caused by one of the pathogens most commonly associated with the disease. Its clinical presentation contrasts to that of "typical" pneumonia. A variety of microorganisms can cause it. When it develops independently from another disease, it is called primary atypical pneumonia (PAP).

Atelectasis is the partial collapse or closure of a lung resulting in reduced or absent gas exchange. It is usually unilateral, affecting part or all of one lung. It is a condition where the alveoli are deflated down to little or no volume, as distinct from pulmonary consolidation, in which they are filled with liquid. It is often referred to informally as a collapsed lung, although more accurately it usually involves only a partial collapse, and that ambiguous term is also informally used for a fully collapsed lung caused by a pneumothorax.
Community-acquired pneumonia (CAP) refers to pneumonia contracted by a person outside of the healthcare system. In contrast, hospital-acquired pneumonia (HAP) is seen in patients who have recently visited a hospital or who live in long-term care facilities. CAP is common, affecting people of all ages, and its symptoms occur as a result of oxygen-absorbing areas of the lung (alveoli) filling with fluid. This inhibits lung function, causing dyspnea, fever, chest pains and cough.
Ventilator-associated pneumonia (VAP) is a type of lung infection that occurs in people who are on mechanical ventilation breathing machines in hospitals. As such, VAP typically affects critically ill persons that are in an intensive care unit (ICU) and have been on a mechanical ventilator for at least 48 hours. VAP is a major source of increased illness and death. Persons with VAP have increased lengths of ICU hospitalization and have up to a 20–30% death rate. The diagnosis of VAP varies among hospitals and providers but usually requires a new infiltrate on chest x-ray plus two or more other factors. These factors include temperatures of >38 °C or <36 °C, a white blood cell count of >12 × 109/ml, purulent secretions from the airways in the lung, and/or reduction in gas exchange.

Respiratory diseases, or lung diseases, are pathological conditions affecting the organs and tissues that make gas exchange difficult in air-breathing animals. They include conditions of the respiratory tract including the trachea, bronchi, bronchioles, alveoli, pleurae, pleural cavity, the nerves and muscles of respiration. Respiratory diseases range from mild and self-limiting, such as the common cold, influenza, and pharyngitis to life-threatening diseases such as bacterial pneumonia, pulmonary embolism, tuberculosis, acute asthma, lung cancer, and severe acute respiratory syndromes, such as COVID-19. Respiratory diseases can be classified in many different ways, including by the organ or tissue involved, by the type and pattern of associated signs and symptoms, or by the cause of the disease.
Bronchoalveolar lavage (BAL), also known as bronchoalveolar washing, is a diagnostic method of the lower respiratory system in which a bronchoscope is passed through the mouth or nose into an appropriate airway in the lungs, with a measured amount of fluid introduced and then collected for examination. This method is typically performed to diagnose pathogenic infections of the lower respiratory airways, though it also has been shown to have utility in diagnosing interstitial lung disease. Bronchoalveolar lavage can be a more sensitive method of detection than nasal swabs in respiratory molecular diagnostics, as has been the case with SARS-CoV-2 where bronchoalveolar lavage samples detect copies of viral RNA after negative nasal swab testing.
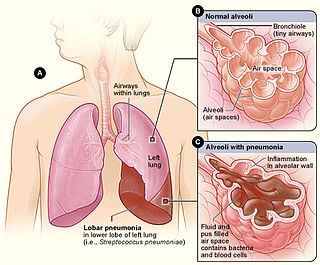
Lobar pneumonia is a form of pneumonia characterized by inflammatory exudate within the intra-alveolar space resulting in consolidation that affects a large and continuous area of the lobe of a lung.

Hospital-acquired pneumonia (HAP) or nosocomial pneumonia refers to any pneumonia contracted by a patient in a hospital at least 48–72 hours after being admitted. It is thus distinguished from community-acquired pneumonia. It is usually caused by a bacterial infection, rather than a virus.
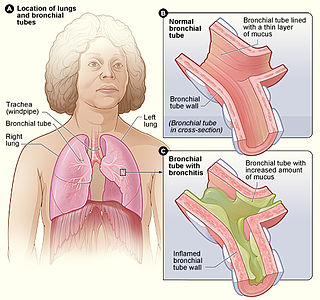
Bronchitis is inflammation of the bronchi in the lungs that causes coughing. Bronchitis usually begins as an infection in the nose, ears, throat, or sinuses. The infection then makes its way down to the bronchi. Symptoms include coughing up sputum, wheezing, shortness of breath, and chest pain. Bronchitis can be acute or chronic.

Tracheobronchial injury is damage to the tracheobronchial tree. It can result from blunt or penetrating trauma to the neck or chest, inhalation of harmful fumes or smoke, or aspiration of liquids or objects.

An acute exacerbation of chronic obstructive pulmonary disease, or acute exacerbations of chronic bronchitis (AECB), is a sudden worsening of chronic obstructive pulmonary disease (COPD) symptoms including shortness of breath, quantity and color of phlegm that typically lasts for several days.

Tracheobronchopathia osteochondroplastica (TO) is a rare benign disease of unknown cause, in which multiple cartilaginous or bony submucosal nodules project into the trachea and proximal bronchi. The nodules usually spare the posterior wall of the airway because they are of cartilaginous origin, while the posterior wall of the airway is membranous (does not contain cartilage). This is as opposed to tracheobronchial amyloidosis, which does not spare the posterior wall.
References
- 1 2 Nseir, S.; Di Pompeo, C.; Pronnier, P.; Beague, S.; Onimus, T.; Saulnier, F.; Grandbastien, B.; Mathieu, D.; Delvallez-Roussel, M.; Durocher, A. (2002). "Nosocomial tracheobronchitis in mechanically ventilated patients: incidence, aetiology and outcome". European Respiratory Journal. 20 (6): 1483–1489. doi: 10.1183/09031936.02.00012902 . PMID 12503708.
- ↑ Sethi, Sanjay (2012). Netter's Infectious Diseases. Elsevier/Saunders. pp. 183–186. ISBN 9781437701265.
- ↑ Craven, D; Chroneou, A (February 2009). "Ventilator-associated tracheobronchitis: the impact of targeted antibiotic therapy on patient outcomes". Chest. 135 (2): 521–528. doi:10.1378/chest.08-1617. PMID 18812452. S2CID 22463384.
- ↑ Craven, D; Hudcova, J (October 2014). "Antibiotic treatment of ventilator-associated tracheobronchitis: to treat or not to treat?". Currently Opin Crit Care. 20 (5): 532–541. doi:10.1097/MCC.0000000000000130. PMID 25051351. S2CID 20457485.
- ↑ Clarke, A; Skelton, J (January 1991). "Fungal tracheobronchitis. Report of 9 cases and review of the literature". Medicine (Baltimore). 70 (1): 1–14. doi: 10.1097/00005792-199101000-00001 . PMID 1988763. S2CID 9964063.
- ↑ Weinberger, Steven; Cockrill, Barbara; Mandell, Jess (2019). Principles of Pulmonary Medicine. Elsevier. p. 120. ISBN 9780323523714.
- ↑ Sethi, Sanjay (2012). Netter's Infectious Diseases. Elsevier/Saunders. pp. 183–186. ISBN 9781437701265.