Related Research Articles

Hypoxia is a condition in which the body or a region of the body is deprived of adequate oxygen supply at the tissue level. Hypoxia may be classified as either generalized, affecting the whole body, or local, affecting a region of the body. Although hypoxia is often a pathological condition, variations in arterial oxygen concentrations can be part of the normal physiology, for example, during strenuous physical exercise.

Shock is the state of insufficient blood flow to the tissues of the body as a result of problems with the circulatory system. Initial symptoms of shock may include weakness, tachycardia, hyperventilation, sweating, anxiety, and increased thirst. This may be followed by confusion, unconsciousness, or cardiac arrest, as complications worsen.

Respiratory failure results from inadequate gas exchange by the respiratory system, meaning that the arterial oxygen, carbon dioxide, or both cannot be kept at normal levels. A drop in the oxygen carried in the blood is known as hypoxemia; a rise in arterial carbon dioxide levels is called hypercapnia. Respiratory failure is classified as either Type 1 or Type 2, based on whether there is a high carbon dioxide level, and can be acute or chronic. In clinical trials, the definition of respiratory failure usually includes increased respiratory rate, abnormal blood gases, and evidence of increased work of breathing. Respiratory failure causes an altered state of consciousness due to ischemia in the brain.

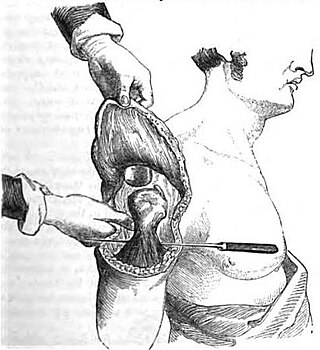
Rhinoplasty, commonly called nose job, medically called nasal reconstruction, is a plastic surgery procedure for altering and reconstructing the nose. There are two types of plastic surgery used – reconstructive surgery that restores the form and functions of the nose and cosmetic surgery that changes the appearance of the nose. Reconstructive surgery seeks to resolve nasal injuries caused by various traumas including blunt, and penetrating trauma and trauma caused by blast injury. Reconstructive surgery can also treat birth defects, breathing problems, and failed primary rhinoplasties. Rhinoplasty may remove a bump, narrow nostril width, change the angle between the nose and the mouth, or address injuries, birth defects, or other problems that affect breathing, such as a deviated nasal septum or a sinus condition. Surgery only on the septum is called a septoplasty.
An arterial blood gas (ABG) test, or arterial blood gas analysis (ABGA) measures the amounts of arterial gases, such as oxygen and carbon dioxide. An ABG test requires that a small volume of blood be drawn from the radial artery with a syringe and a thin needle, but sometimes the femoral artery in the groin or another site is used. The blood can also be drawn from an arterial catheter.

Peripheral artery disease (PAD) is a vascular disorder that causes abnormal narrowing of arteries other than those that supply the heart or brain. PAD can happen in any blood vessel, but it is more common in the legs than the arms.

Intracranial pressure (ICP) is the pressure exerted by fluids such as cerebrospinal fluid (CSF) inside the skull and on the brain tissue. ICP is measured in millimeters of mercury (mmHg) and at rest, is normally 7–15 mmHg for a supine adult. This equals to 9–20 cmH2O, which is a common scale used in lumbar punctures. The body has various mechanisms by which it keeps the ICP stable, with CSF pressures varying by about 1 mmHg in normal adults through shifts in production and absorption of CSF.

Hypovolemic shock is a form of shock caused by severe hypovolemia. It can be caused by severe dehydration or blood loss. Hypovolemic shock is a medical emergency; if left untreated, the insufficient blood flow can cause damage to organs, leading to multiple organ failure.

Cardiac catheterization is the insertion of a catheter into a chamber or vessel of the heart. This is done both for diagnostic and interventional purposes.
Hyperoxia is the state of being exposed to high levels of oxygen; it may refer to organisms, cells and tissues that are experiencing excessive oxygenation, or to an abnormally high oxygen concentration in an environment.
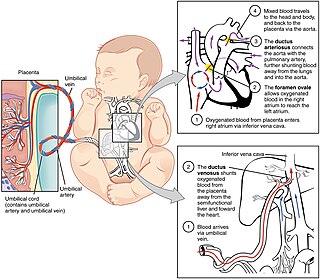
In humans, the circulatory system is different before and after birth. The fetal circulation is composed of the placenta, umbilical blood vessels encapsulated by the umbilical cord, heart and systemic blood vessels. A major difference between the fetal circulation and postnatal circulation is that the lungs are not used during the fetal stage resulting in the presence of shunts to move oxygenated blood and nutrients from the placenta to the fetal tissue. At birth, the start of breathing and the severance of the umbilical cord prompt various changes that quickly transform fetal circulation into postnatal circulation.
A chronic wound is a wound that does not progress through the normal stages of wound healing—haemostasis, inflammation, proliferation, and remodeling—in a predictable and timely manner. Typically, wounds that do not heal within three months are classified as chronic. Chronic wounds may remain in the inflammatory phase due to factors like infection or bacterial burden, ischaemia, presence of necrotic tissue, improper moisture balance of wound site, or underlying diseases such as diabetes mellitus.

Calciphylaxis, also known as calcific uremic arteriolopathy (CUA) or “Grey Scale”, is a rare syndrome characterized by painful skin lesions. The pathogenesis of calciphylaxis is unclear but believed to involve calcification of the small blood vessels located within the fatty tissue and deeper layers of the skin, blood clots, and eventual death of skin cells due to lack of blood flow. It is seen mostly in people with end-stage kidney disease but can occur in the earlier stages of chronic kidney disease and rarely in people with normally functioning kidneys. Calciphylaxis is a rare but serious disease, believed to affect 1-4% of all dialysis patients. It results in chronic non-healing wounds and indicates poor prognosis, with typical life expectancy of less than one year.
A pulmonary shunt is the passage of deoxygenated blood from the right side of the heart to the left without participation in gas exchange in the pulmonary capillaries. It is a pathological condition that results when the alveoli of parts of the lungs are perfused with blood as normal, but ventilation fails to supply the perfused region. In other words, the ventilation/perfusion ratio of those areas is zero.
The Alveolar–arterial gradient, is a measure of the difference between the alveolar concentration (A) of oxygen and the arterial (a) concentration of oxygen. It is a useful parameter for narrowing the differential diagnosis of hypoxemia.

Lutembacher's syndrome is a very rare form of congenital heart disease that affects one of the chambers of the heart as well as a valve. It is commonly known as both congenital atrial septal defect (ASD) and acquired mitral stenosis (MS). Congenital atrial septal defect refers to a hole being in the septum or wall that separates the two atria; this condition is usually seen in fetuses and infants. Mitral stenosis refers to mitral valve leaflets sticking to each other making the opening for blood to pass from the atrium to the ventricles very small. With the valve being so small, blood has difficulty passing from the left atrium into the left ventricle. Septal defects that may occur with Lutembacher's syndrome include: Ostium primum atrial septal defect or ostium secundum which is more prevalent.
Flap surgery is a technique in plastic and reconstructive surgery where tissue with an intact blood supply is lifted from a donor site and moved to a recipient site. Flaps are distinct from grafts, which do not have an intact blood supply and relies on the growth of new blood vessels. Flaps are done to fill a defect such as a wound resulting from injury or surgery when the remaining tissue is unable to support a graft, wound contraction is to be avoided or to rebuild more complex anatomic structures like breasts or jaws. Flaps may also carry with them tissues such as muscle and bone that may be useful in the ultimate reconstruction.
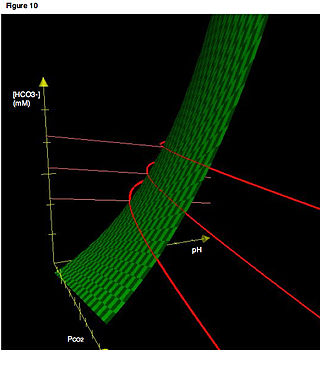
Blood gas tension refers to the partial pressure of gases in blood. There are several significant purposes for measuring gas tension. The most common gas tensions measured are oxygen tension (PxO2), carbon dioxide tension (PxCO2) and carbon monoxide tension (PxCO). The subscript x in each symbol represents the source of the gas being measured: "a" meaning arterial, "A" being alveolar, "v" being venous, and "c" being capillary. Blood gas tests (such as arterial blood gas tests) measure these partial pressures.
Chronic limb threatening ischemia (CLTI), also known as critical limb ischemia (CLI), is an advanced stage of peripheral artery disease (PAD). It is defined as ischemic rest pain, arterial insufficiency ulcers, and gangrene. The latter two conditions are jointly referred to as tissue loss, reflecting the development of surface damage to the limb tissue due to the most severe stage of ischemia. Compared to the other manifestation of PAD, intermittent claudication, CLI has a negative prognosis within a year after the initial diagnosis, with 1-year amputation rates of approximately 12% and mortality of 50% at 5 years and 70% at 10 years.

Nerve entrapment involves a cascade of physiological changes caused by compression and tension. Some of these changes are irreversible. The magnitude and duration of the forces determines the extent of injury. In the acute form, mechanical injury and metabolic blocks impede nerve function. In the chronic form, there is a sequence of changes starting with a breakdown of the blood-nerve-barrier, followed by edema with connective tissue changes, followed by diffuse demyelination, and finally followed by axonmetesis. The injury will often be a mixed lesion where mild/moderate compression is a combination of a metabolic block and neuropraxia, while severe compression combines elements of neuropraxia and axonmetesis.
References
- 1 2 Arsenault KA, McDonald J, Devereaux PJ, Thorlund K, Tittley JG, Whitlock RP (2011). "The use of transcutaneous oximetry to predict complications of chronic wound healing: a systematic review and meta-analysis". Wound Repair Regen. 19 (6): 657–63. doi:10.1111/j.1524-475X.2011.00731.x. PMID 22092835. S2CID 30522546.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Byrne P, Provan JL, Ameli FM, Jones DP (1984). "The use of transcutaneous oxygen tension measurements in the diagnosis of peripheral vascular insufficiency". Ann Surg. 200 (2): 159–65. doi:10.1097/00000658-198408000-00007. PMC 1250438 . PMID 6465970.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Bowers BL, Valentine RJ, Myers SI, Chervu A, Clagett GP (1993). "The natural history of patients with claudication with toe pressures of 40 mm Hg or less". J Vasc Surg. 18 (3): 506–11. doi:10.1016/0741-5214(93)90269-R. PMID 8377245.
{{cite journal}}: CS1 maint: multiple names: authors list (link)