Lichen planus (LP) is a chronic inflammatory and immune-mediated disease that affects the skin, nails, hair, and mucous membranes. It is not an actual lichen, and is only named that because it looks like one. It is characterized by polygonal, flat-topped, violaceous papules and plaques with overlying, reticulated, fine white scale, commonly affecting dorsal hands, flexural wrists and forearms, trunk, anterior lower legs and oral mucosa. Although there is a broad clinical range of LP manifestations, the skin and oral cavity remain as the major sites of involvement. The cause is unknown, but it is thought to be the result of an autoimmune process with an unknown initial trigger. There is no cure, but many different medications and procedures have been used in efforts to control the symptoms.

{{Drugbox | Verifiedfields = changed | Watchedfields = changed | verifiedrevid = 464206673 | IUPAC_name = (3S,4R,5S,8R,9E,12S,14S,15R,16S,18R,19R,26aS)-3-{(E)-2-[(1R,3R,4S)-4-chloro-3 -methoxycyclohexyl]-1-methylvinyl}-8-ethyl-5,6,8,11,12,13,14,15,16,17,18,19,24,25,26,26a-hexadecahydro-5,19-dihydroxy-14,16-dimethoxy-4,10,12,18-tetramethyl-15,19-epoxy-3H-pyrido[2,1-c][1,4]oxaazacyclotricosin-1,7,20,21(4H,23H)-tetrone | image = Pimecrolimus2DACS.svg | width = 200 | image2 = Pimecrolimus ball-and-stick.png | tradename = Elidel | Drugs.com = Monograph | pregnancy_AU = B3 | pregnancy_US = C | legal_US = Rx-only | routes_of_administration = topical | bioavailability = low systemic absorption | protein_bound = 74%–87% | metabolism = Hepatic CYP3A | elimination_half-life = | excretion = | CAS_number_Ref = | CAS_number = 137071-32-0 | ATC_prefix = D11 | ATC_suffix = AH02 | PubChem = 16051947 | DrugBank_Ref =
| DrugBank = DB00337
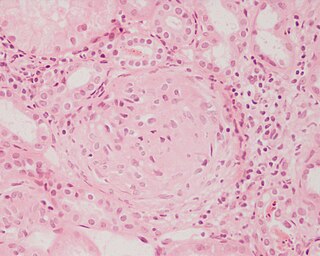
Libman–Sacks endocarditis (LSE) is a form of non-bacterial endocarditis that is seen in association with systemic lupus erythematosus (SLE), antiphospholipid syndrome, and malignancies. It is one of the most common heart-related manifestations of lupus.
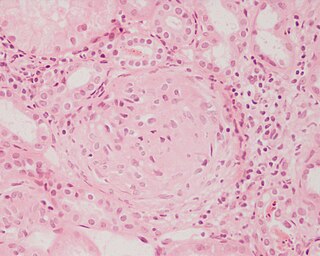
Glomerulonephritis (GN) is a term used to refer to several kidney diseases. Many of the diseases are characterised by inflammation either of the glomeruli or of the small blood vessels in the kidneys, hence the name, but not all diseases necessarily have an inflammatory component.
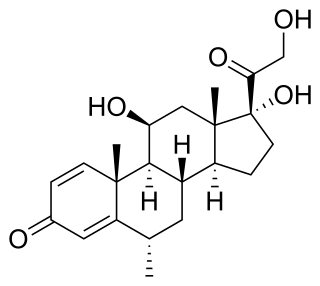
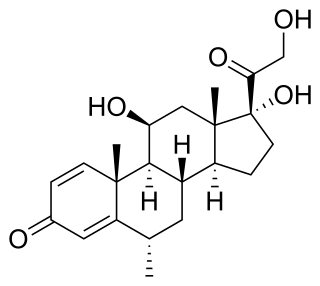
Methylprednisolone is a synthetic glucocorticoid, primarily prescribed for its anti-inflammatory and immunosuppressive effects. It is either used at low doses for chronic illnesses or used concomitantly at high doses during acute flares. Methylprednisolone and its derivatives can be administered orally or parenterally.

Desonide (INN) is a low-potency topical corticosteroid anti-inflammatory that has been available since the 1970s. It is primarily used to treat atopic dermatitis (eczema), seborrheic dermatitis, contact dermatitis and psoriasis in both adults and children. It has a fairly good safety profile and is available as a cream, ointment, lotion, and as a foam under the tradename Verdeso Foam. Other trade names for creams, lotions, and ointments include Tridesilon, DesOwen, Desonate. It is a group VI corticosteroid under US classification, the second least potent group.
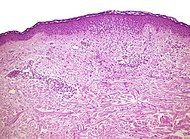
Discoid lupus erythematosus (DLE) is an uncommon autoimmune disease of the basal cell layer of the skin. It occurs in humans and cats, more frequently occurring in dogs. It was first described in dogs by Griffin and colleagues in 1979. DLE is one form of cutaneous lupus erythematosus (CLE). DLE occurs in dogs in two forms: a classical facial predominant form or generalized with other areas of the body affected. Other non-discoid variants of CLE include vesicular CLE, exfoliative CLE and mucocutaenous CLE. It does not progress to systemic lupus erythematosus (SLE) in dogs. SLE can also have skin symptoms, but it appears that the two are either separate diseases. DLE in dogs differs from SLE in humans in that plasma cells predominate histologically instead of T lymphocytes. Because worsening of symptoms occurs with increased ultraviolet light exposure, sun exposure most likely plays a role in DLE, although certain breeds are predisposed. After pemphigus foliaceus, DLE is the second most common autoimmune skin disease in dogs.
A systemic disease is one that affects a number of organs and tissues, or affects the body as a whole.

Cheilitis is a medical condition characterized by inflammation of the lips. According to its onset and course, cheilitis can be either acute or chronic. Most cheilitis is caused by acute sun exposure. Allergic tests may identify allergens that cause cheilitis.

Drug-induced lupus erythematosus is an autoimmune disorder caused by chronic use of certain drugs. These drugs cause an autoimmune response producing symptoms similar to those of systemic lupus erythematosus (SLE). There are 38 known medications to cause DIL but there are three that report the highest number of cases: hydralazine, procainamide, and quinidine. While the criteria for diagnosing DIL has not been thoroughly established, symptoms of DIL typically present as muscle pain and joint pain. Generally, the symptoms recede after discontinuing use of the drugs.

Discoid lupus erythematosus is the most common type of chronic cutaneous lupus (CCLE), an autoimmune skin condition on the lupus erythematosus spectrum of illnesses. It presents with red, inflamed, coin-shaped patches of skin with a scaling and crusty appearance, most often on the scalp, cheeks, and ears. Hair loss may occur if the lesions are on the scalp. The lesions can then develop severe scarring, and the centre areas may appear lighter in color with a rim darker than the normal skin. These lesions can last for years without treatment.

Lupus erythematosus is a collection of autoimmune diseases in which the human immune system becomes hyperactive and attacks healthy tissues. Symptoms of these diseases can affect many different body systems, including joints, skin, kidneys, blood cells, heart, and lungs. The most common and most severe form is systemic lupus erythematosus.

Dermatitis herpetiformis (DH) is a chronic autoimmune blistering skin condition, characterised by blisters filled with a watery fluid that is intensely itchy. DH is a cutaneous manifestation of coeliac disease. DH is neither related to nor caused by herpes virus: the name means that it is a skin inflammation having an appearance similar to herpes.

An autoimmune disease is a condition arising from an abnormal immune response to a functioning body part. There are at least 80 types of autoimmune diseases. Nearly any body part can be involved. Common symptoms include low grade fever and feeling tired. Often symptoms come and go.
Subacute cutaneous lupus erythematosus is a clinically distinct subset of cases of lupus erythematosus that is most often present in white women aged 15 to 40, consisting of skin lesions that are scaly and evolve as poly-cyclic annular lesions or plaques similar to those of plaque psoriasis.

Lupus, technically known as systemic lupus erythematosus (SLE), is an autoimmune disease in which the body's immune system mistakenly attacks healthy tissue in many parts of the body. Symptoms vary between people and may be mild to severe. Common symptoms include painful and swollen joints, fever, chest pain, hair loss, mouth ulcers, swollen lymph nodes, feeling tired, and a red rash which is most commonly on the face. Often there are periods of illness, called flares, and periods of remission during which there are few symptoms.
Acute cutaneous lupus erythematosus is a cutaneous condition characterized by a bilateral malar rash and lesions that tend to be transient, and that follow sun exposure. The acute form is distinct from chronic and subacute cutaneous lupus erythematosus, which may have different types of skin lesions. Cutaneous lupus erythematosus is associated with both lupus erythematosus-specific lesions and cutaneous manifestations that are not specific to lupus erythematosus, such as oral ulcers and urticaria. Because of the diagnostic criteria used to diagnose systemic lupus erythematosus, a patient with only cutaneous manifestations may be diagnosed with the systemic form of the disease.

Anti-SSA autoantibodies are a type of anti-nuclear autoantibodies that are associated with many autoimmune diseases, such as systemic lupus erythematosus (SLE), SS/SLE overlap syndrome, subacute cutaneous lupus erythematosus (SCLE), neonatal lupus and primary biliary cirrhosis. They are often present in Sjögren's syndrome (SS). Additionally, Anti-Ro/SSA can be found in other autoimmune diseases such as systemic sclerosis (SSc), polymyositis/dermatomyositis (PM/DM), rheumatoid arthritis (RA), and mixed connective tissue disease (MCTD), and are also associated with heart arrhythmia.
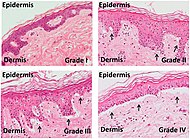
Histopathology of dermatitis can be performed in uncertain cases of inflammatory skin condition that remain uncertain after history and physical examination.