Skin is the layer of usually soft, flexible outer tissue covering the body of a vertebrate animal, with three main functions: protection, regulation, and sensation.

The integumentary system is the set of organs forming the outermost layer of an animal's body. It comprises the skin and its appendages, which act as a physical barrier between the external environment and the internal environment that it serves to protect and maintain the body of the animal. Mainly it is the body's outer skin.

Epithelium or epithelial tissue is a thin, continuous, protective layer of compactly packed cells with a little intercellular matrix. Epithelial tissues line the outer surfaces of organs and blood vessels throughout the body, as well as the inner surfaces of cavities in many internal organs. An example is the epidermis, the outermost layer of the skin. Epithelial tissue is one of the four basic types of animal tissue, along with connective tissue, muscle tissue and nervous tissue.

Keratinocytes are the primary type of cell found in the epidermis, the outermost layer of the skin. In humans, they constitute 90% of epidermal skin cells. Basal cells in the basal layer of the skin are sometimes referred to as basal keratinocytes. Keratinocytes form a barrier against environmental damage by heat, UV radiation, water loss, pathogenic bacteria, fungi, parasites, and viruses. A number of structural proteins, enzymes, lipids, and antimicrobial peptides contribute to maintain the important barrier function of the skin. Keratinocytes differentiate from epidermal stem cells in the lower part of the epidermis and migrate towards the surface, finally becoming corneocytes and eventually be shed off, which happens every 40 to 56 days in humans.
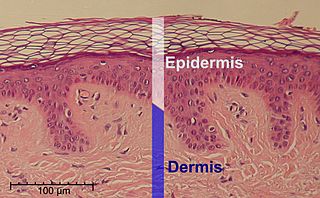
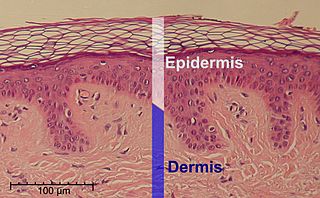
The epidermis is the outermost of the three layers that comprise the skin, the inner layers being the dermis and hypodermis. The epidermis layer provides a barrier to infection from environmental pathogens and regulates the amount of water released from the body into the atmosphere through transepidermal water loss.

The dermis or corium is a layer of skin between the epidermis and subcutaneous tissues, that primarily consists of dense irregular connective tissue and cushions the body from stress and strain. It is divided into two layers, the superficial area adjacent to the epidermis called the papillary region and a deep thicker area known as the reticular dermis. The dermis is tightly connected to the epidermis through a basement membrane. Structural components of the dermis are collagen, elastic fibers, and extrafibrillar matrix. It also contains mechanoreceptors that provide the sense of touch and thermoreceptors that provide the sense of heat. In addition, hair follicles, sweat glands, sebaceous glands, apocrine glands, lymphatic vessels, nerves and blood vessels are present in the dermis. Those blood vessels provide nourishment and waste removal for both dermal and epidermal cells.

A skin condition, also known as cutaneous condition, is any medical condition that affects the integumentary system—the organ system that encloses the body and includes skin, nails, and related muscle and glands. The major function of this system is as a barrier against the external environment.

The basement membrane, also known as base membrane is a thin, pliable sheet-like type of extracellular matrix that provides cell and tissue support and acts as a platform for complex signalling. The basement membrane sits between epithelial tissues including mesothelium and endothelium, and the underlying connective tissue.

Bullous pemphigoid is an autoimmune pruritic skin disease which typically occurs in people aged over 60, that may involve the formation of blisters (bullae) in the space between the epidermal and dermal skin layers. It is classified as a type II hypersensitivity reaction, which involves formation of anti-hemidesmosome antibodies, causing a loss of keratinocytes to basement membrane adhesion.

Vacuolization is the formation of vacuoles or vacuole-like structures, within or adjacent to cells. Perinuclear vacuolization of epidermal keratinocytes is most likely inconsequential when not observed in combination with other pathologic findings. In dermatopathology "vacuolization" often refers specifically to vacuoles in the basal cell-basement membrane zone area, where it is an unspecific sign of disease. It may be a sign of for example vacuolar interface dermatitis, which in turn has many causes.

Pemphigoid is a group of rare autoimmune blistering diseases of the skin, and mucous membranes. As its name indicates, pemphigoid is similar in general appearance to pemphigus, but, unlike pemphigus, pemphigoid does not feature acantholysis, a loss of connections between skin cells.

Collagen alpha-1(VII) chain is a protein that in humans is encoded by the COL7A1 gene. It is composed of a triple helical, collagenous domain flanked by two non-collagenous domains, and functions as an anchoring fibril between the dermal-epidermal junction in the basement membrane. Mutations in COL7A1 cause all types of dystrophic epidermolysis bullosa, and the exact mutations vary based on the specific type or subtype. It has been shown that interactions between the NC-1 domain of collagen VII and several other proteins, including laminin-5 and collagen IV, contribute greatly to the overall stability of the basement membrane.
Anchoring fibrils extend from the basal lamina of epithelial cells and attach to the lamina reticularis by wrapping around the reticular fiber bundles. The basal lamina and lamina reticularis together make up the basement membrane. Anchoring fibrils are essential to the functional integrity of the dermoepidermal junction.

Dermatitis herpetiformis (DH) is a chronic autoimmune blistering skin condition, characterised by intensely itchy blisters filled with a watery fluid. DH is a cutaneous manifestation of coeliac disease, although the exact causal mechanism is not known. DH is neither related to nor caused by herpes virus; the name means that it is a skin inflammation having an appearance similar to herpes.
Epidermolysis bullosa acquisita, also known as acquired epidermolysis bullosa, is a longterm autoimmune blistering skin disease. It generally presents with fragile skin that blisters and becomes red with or without trauma. Marked scarring is left with thin skin, milia and nail changes. It typically begins around age 50.
Paraneoplastic pemphigus (PNP) is an autoimmune disorder stemming from an underlying tumor. It is hypothesized that antigens associated with the tumor trigger an immune response resulting in blistering of the skin and mucous membranes.
Junctional epidermolysis bullosa is a skin condition characterized by blister formation within the lamina lucida of the basement membrane zone.
Nevus cells are a variant of melanocytes. They are larger than typical melanocytes, do not have dendrites, and have more abundant cytoplasm with coarse granules. They are usually located at the dermoepidermal junction or in the dermis of the skin. Dermal nevus cells can be further classified: type A (epithelioid) dermal nevus cells mature into type B (lymphocytoid) dermal nevus cells which mature further into type C (neuroid) dermal nevus cells, through a process involving downwards migration.
Histopathology of dermatitis can be performed in uncertain cases of inflammatory skin condition that remain uncertain after history and physical examination.