The management of HIV/AIDS normally includes the use of multiple antiretroviral drugs as a strategy to control HIV infection. There are several classes of antiretroviral agents that act on different stages of the HIV life-cycle. The use of multiple drugs that act on different viral targets is known as highly active antiretroviral therapy (HAART). HAART decreases the patient's total burden of HIV, maintains function of the immune system, and prevents opportunistic infections that often lead to death. HAART also prevents the transmission of HIV between serodiscordant same-sex and opposite-sex partners so long as the HIV-positive partner maintains an undetectable viral load.

Nevirapine (NVP), sold under the brand name Viramune among others, is a medication used to treat and prevent HIV/AIDS, specifically HIV-1. It is generally recommended for use with other antiretroviral medications. It may be used to prevent mother to child spread during birth but is not recommended following other exposures. It is taken by mouth.
Following infection with HIV-1, the rate of clinical disease progression varies between individuals. Factors such as host susceptibility, genetics and immune function, health care and co-infections as well as viral genetic variability may affect the rate of progression to the point of needing to take medication in order not to develop AIDS.
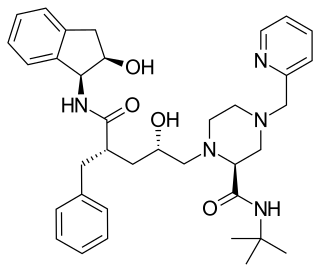
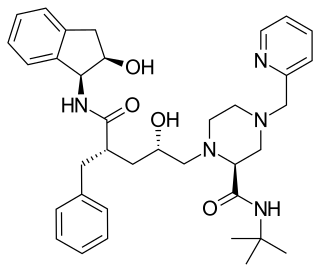
Indinavir is a protease inhibitor used as a component of highly active antiretroviral therapy to treat HIV/AIDS. It is soluble white powder administered orally in combination with other antiviral drugs. The drug prevents protease from functioning normally. Consequently, HIV viruses cannot reproduce, causing a decrease in the viral load. Commercially sold indinavir is indinavir anhydrous, which is indinavir with an additional amine in the hydroxyethylene backbone. This enhances its solubility and oral bioavailability, making it easier for users to intake. It was synthetically produced for the purpose of inhibiting the protease in the HIV virus.
The Division of Acquired Immunodeficiency Syndrome (DAIDS) is a division of the National Institute of Allergy and Infectious Diseases, which is part of the National Institutes of Health. It was formed in 1986 as a part of the initiative to address the national research needs created by the advent and spread of the HIV/AIDS epidemic. Specifically, the Division's mission is to increase basic knowledge of the pathogenesis, natural history, and transmission of HIV disease and to support research that promotes progress in its detection, treatment, and prevention. DAIDS accomplishes this through planning, implementing, managing, and evaluating programs in (1) fundamental basic research, (2) discovery and development of therapies for HIV infection and its complications, and (3) discovery and development of vaccines and other prevention strategies.

Infection with HIV, a retrovirus, can be managed with treatment but without treatment can lead to a spectrum of conditions including AIDS.
Douglas D. Richman is an American infectious diseases physician and medical virologist. Richman's work has focused on the HIV/AIDS pandemic, since its appearance in the early 1980s. His major contributions have been in the areas of treatment, drug resistance, and pathogenicity.
Long-term nonprogressors (LTNPs), are individuals infected with HIV, who maintain a CD4 count greater than 500 without antiretroviral therapy with a detectable viral load. Many of these patients have been HIV positive for 30 years without progressing to the point of needing to take medication in order not to develop AIDS. They have been the subject of a great deal of research, since an understanding of their ability to control HIV infection may lead to the development of immune therapies or a therapeutic vaccine. The classification "Long-term non-progressor" is not permanent, because some patients in this category have gone on to develop AIDS.
Vedolizumab, sold under the brand name Entyvio, is a monoclonal antibody medication developed by Millennium Pharmaceuticals, Inc. for the treatment of ulcerative colitis and Crohn's disease. It binds to integrin α4β7, blocking the α4β7 integrin results in gut-selective anti-inflammatory activity.
HIV drug resistance occurs when microevolution causes virions to become tolerant to antiretroviral treatments (ART). ART can be used to successfully manage HIV infection, but a number of factors can contribute to the virus mutating and becoming resistant. Drug resistance occurs as bacterial or viral populations evolve to no longer respond to medications that previously worked. In the case of HIV, there have been recognized cases of treatment resistant strains since 1989, with drug resistance being a major contributor to treatment failure. While global incidence varies greatly from region to region, there has been a general increase in overall HIV drug resistance. The two main types of resistance, primary and induced, differ mostly in causation, with the biggest cause of resistance being a lack of adherence to the specific details of treatment. These newly created resistant strains of HIV pose a public health issue as they infect a growing number of people because they are harder to treat, and can be spread to other individuals. For this reason, the reaction to the growing number of cases of resistant HIV strains has mostly been to try to increase access to treatment and implement other measures to make sure people stay in care, as well as to look into the development of an HIV vaccine or cure.
AntiViral-HyperActivation Limiting Therapeutics (AV-HALTs) are an investigational class of antiretroviral drugs used to treat Human Immunodeficiency Virus (HIV) infection. Unlike other antiretroviral agents given to reduce viral replication, AV-HALTs are single or combination drugs designed to reduce the rate of viral replication while, at the same time, also directly reducing the state of immune system hyperactivation now believed to drive the loss of CD4+ T helper cells leading to disease progression and Acquired Immunodeficiency Syndrome (AIDS).
HIV Resistance Response Database Initiative (RDI) is a not-for-profit organisation established in 2002 which states its mission as "To improve the clinical management of HIV infection by developing a large clinical database and bioinformatic techniques that predict accurately any individual's response to any combination of HIV drugs."
The Berlin patient is an anonymous person from Berlin, Germany, who was described in 1998 as exhibiting prolonged "post-treatment control" of HIV viral load after HIV treatments were interrupted.

HIV/AIDS research includes all medical research that attempts to prevent, treat, or cure HIV/AIDS, as well as fundamental research about the nature of HIV as an infectious agent and AIDS as the disease caused by HIV.
Julio S. G. Montaner, is an Argentine-Canadian physician, professor and researcher. He is the director of the British Columbia Centre for Excellence in HIV/AIDS, the chair in AIDS Research and head of the Division of AIDS in the Faculty of Medicine at the University of British Columbia and the past-president of the International AIDS Society. He is also the director of the John Ruedy Immunodeficiency Clinic, and the Physician Program Director for HIV/AIDS PHC. He is known for his work on HAART, a role in the discovery of triple therapy as an effective treatment for HIV in the late 1990s, and a role in advocating the "Treatment as Prevention" Strategy in the mid-2000s, led by Myron Cohen of the HPTN 052 trial.
Deborah Persaud is a Guyanese-born American virologist who primarily works on HIV/AIDS at Johns Hopkins Children's Center.
HIV in pregnancy is the presence of an HIV/AIDS infection in a woman while she is pregnant. There is a risk of HIV transmission from mother to child in three primary situations: pregnancy, childbirth, and while breastfeeding. This topic is important because the risk of viral transmission can be significantly reduced with appropriate medical intervention, and without treatment HIV/AIDS can cause significant illness and death in both the mother and child. This is exemplified by data from The Centers for Disease Control (CDC): In the United States and Puerto Rico between the years of 2014–2017, where prenatal care is generally accessible, there were 10,257 infants in the United States and Puerto Rico who were exposed to a maternal HIV infection in utero who did not become infected and 244 exposed infants who did become infected.
Treatment as prevention (TasP) is a concept in public health that promotes treatment as a way to prevent and reduce the likelihood of HIV illness, death and transmission from an infected individual to others. Expanding access to earlier HIV diagnosis and treatment as a means to address the global epidemic by preventing illness, death and transmission was first proposed in 2000 by Garnett et al. The term is often used to talk about treating people that are currently living with human immunodeficiency virus (HIV) and acquired immune deficiency syndrome (AIDS) to prevent illness, death and transmission. Although some experts narrow this to only include preventing infections, treatment prevents illnesses such as tuberculosis and has been shown to prevent death. In relation to HIV, antiretroviral therapy (ART) is a three or more drug combination therapy that is used to decrease the viral load, or the measured amount of virus, in an infected individual. Such medications are used as a preventative for infected individuals to not only spread the HIV virus to their negative partners but also improve their current health to increase their lifespans. When taken correctly, ART is able to diminish the presence of the HIV virus in the bodily fluids of an infected person to a level of undetectability. Consistent adherence to an ARV regimen, monitoring, and testing are essential for continued confirmed viral suppression. Treatment as prevention rose to great prominence in 2011, as part of the HPTN 052 study, which shed light on the benefits of early treatment for HIV positive individuals.
Viral load monitoring for HIV is the regular measurement of the viral load of individual HIV-positive people as part of their personal plan for treatment of HIV/AIDS. A count of the viral load is routine before the start of HIV treatment.

Cabotegravir/rilpivirine, sold under the brand name Cabenuva, is a co-packaged antiretroviral medication for the treatment of HIV/AIDS. It contains cabotegravir and rilpivirine in a package with two separate injection vials.