Related Research Articles
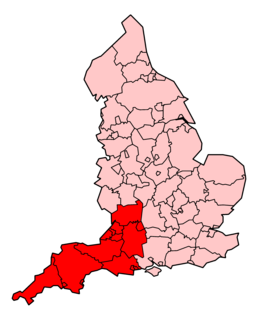
The South Western Ambulance Service NHS Foundation Trust (SWASFT) is the organisation responsible for providing ambulance services for the National Health Service (NHS) across South West England. It serves the council areas of Bath and North East Somerset, Bournemouth, Christchurch and Poole Council, Bristol, Cornwall, Devon, Dorset, Gloucestershire, North Somerset, Plymouth, Isles of Scilly, Somerset, South Gloucestershire, Swindon, Torbay and Wiltshire. On 1 March 2011, SWASFT was the first ambulance service in the country to become a NHS foundation trust. On 1 February 2013, neighbouring Great Western Ambulance Service merged with the trust.
Healthcare in the UK is mainly provided by the National Health Service, a public body that provides healthcare to all permanent residents of the United Kingdom that is free at the point of use and paid for from general taxation. Since health is a devolved matter, there are differences with the provisions for healthcare elsewhere in the United Kingdom. Though the public system dominates healthcare provision in England, private health care and a wide variety of alternative and complementary treatments are available for those willing to pay.

111 is a free-to-call single non-emergency number medical helpline operating in England, Scotland and parts of Wales. The 111 phone service has replaced the various non-geographic 0845 rate numbers and is part of each country's National Health Service: in England the service is known as NHS 111; in Scotland, NHS 24; and in Wales, either NHS Direct Wales or 111 depending on area.

Care UK is a British company providing health and social care. The company works with councils, Clinical Commissioning Groups and doctors to deliver care and support for older people and those with learning disabilities or mental health problems, as well as a range of healthcare services for NHS patients.

Virgin Care is a private provider of publicly funded community health and social services, and has been commissioned by the National Health Service and Local Authorities in England since 2010.

NHS Pathways is a triage software utilised by the National Health Service of England to triage public telephone calls for medical care and emergency medical services – such as 999 or 111 calls – in some NHS trusts and five of the ambulance services in the country. In its emergency capacity, it has replaced the Advanced Medical Priority Dispatch System for some trusts, and in non-emergency telephone triage it is found in many medical care triage systems, such as NHS 111.
The Hurley Group is a large provider of primary care services in London, one of only 3 organisations in England which served more than 100,000 patients in 2014. In 2012 it ran 13 practices, had 250 employees and provided a variety of NHS services across London.
Fylde Coast Medical Services is a provider of Out of Hours medical services for the Blackpool, Fylde and Wyre areas.
York Teaching Hospital NHS Foundation Trust runs York Hospital, Archways Community Intermediate Care Inpatient Facility, St Helen's Rehabilitation Hospital and White Cross Court Rehabilitation Hospital in York, Bridlington Hospital, St Monica’s Easingwold, New Selby War Memorial Hospital and Scarborough General Hospital.
Out-of-hours services are the arrangements to provide access to healthcare at times when General Practitioner surgeries are closed; in the United Kingdom this is normally between 6.30pm and 8am, at weekends, at Bank Holidays and sometimes if the practice is closed for educational sessions.
The Five Year Forward View was produced by NHS England in October 2014 under the leadership of Simon Stevens as a planning document.
Healthcare in Kent is now mainly the responsibility from 1st April 2020 of the Kent & Medway Clinical Commissioning Group. Certain specialised services are directly commissioned by NHS England, coordinated through the South East integrated regional team. Some NHS England structures are aligned on a Kent & Medway basis, others on a South East basis and there is liaison with London that provides many tertiary healthcare services to the residents of Kent.
Healthcare in Somerset, England is the responsibility of three clinical commissioning groups (CCGs) covering the county of Somerset, and the unitary authorities of North Somerset and Bath and North East Somerset.
Healthcare in Cornwall, United Kingdom, is now the responsibility of Kernow clinical commissioning group, a National Health Service (NHS) organisation set up by the Health and Social Care Act 2012 to organise the delivery of NHS services in England. As far as the NHS is concerned, Cornwall includes the Isles of Scilly.
Healthcare in the West Midlands is now the responsibility of five clinical commissioning groups (CCG): Birmingham and Solihull; Sandwell and West Birmingham; Dudley; Wolverhampton; and Walsall.
Healthcare in Suffolk is now the responsibility of two clinical commissioning groups: Ipswich and East Suffolk, and West Suffolk.
Harmoni was a provider of outsourced healthcare services including Out-of-hours services, NHS 111, prisoner healthcare and IT services. It provided NHS services to more than eight million people in the UK.
Healthcare in Northumberland, since 2013, is the responsibility of the Northumberland, Newcastle Gateshead and North Tyneside clinical commissioning groups.
Healthcare in Shropshire is now the responsibility of two clinical commissioning groups: Shropshire, and Telford and Wrekin
GP Federations became popular among English general practitioners after 2010 as a means to exploit the opportunities - or mitigate the threats - posed by the Five Year Forward View proposals in the English NHS which envisaged delivering primary care at a larger scale than the traditional GP list. It is widely believed that ‘Practices cannot survive on their own – they have to look at ways of making themselves stronger.’ 15 sites were selected in December 2015 to test new enhanced primary care models serving populations of 30,000 to 50,000 patients. Some, but by no means all, clinical commissioning groups have given financial support to encourage the formation of federations.
References
- ↑ "Vocare expand into new Balliol Business Park HQ in Newcastle as turnover soars 52%". Chronicle Live. 6 October 2015. Retrieved 16 July 2017.
- ↑ "New operator for NHS 111 service in Shropshire". Shropshire Star. 6 July 2015. Retrieved 16 July 2017.
- ↑ "New NHS-private partnership wins £48m contract". Health Service Journal. 23 June 2017. Retrieved 16 July 2017.
- ↑ "Health centres ordered to improve by Government inspectors". Sunderland Echo. 17 May 2017. Retrieved 16 July 2017.
- ↑ "Nissan takes crown as the North East's largest company in Journal's Top 200 event". Chronicle Live. 15 November 2016. Retrieved 23 June 2019.
- ↑ "Out of hours care provider bought for £11m". Health Service Journal. 24 November 2017. Retrieved 31 December 2017.
- ↑ "Plans drawn up to partially privatise York A&E, say MP and staff". York Press. 2 March 2021. Retrieved 2 March 2021.