Related Research Articles

The perineum in humans is the space between the anus and scrotum in the male, or between the anus and the vulva in the female. The perineum is the region of the body between the pubic symphysis and the coccyx, including the perineal body and surrounding structures. There is some variability in how the boundaries are defined. The perineal raphe is visible and pronounced to varying degrees. The perineum is an erogenous zone.

Fecal incontinence (FI), or in some forms encopresis, is a lack of control over defecation, leading to involuntary loss of bowel contents, both liquid stool elements and mucus, or solid feces. When this loss includes flatus (gas), it is referred to as anal incontinence. FI is a sign or a symptom, not a diagnosis. Incontinence can result from different causes and might occur with either constipation or diarrhea. Continence is maintained by several interrelated factors, including the anal sampling mechanism, and incontinence usually results from a deficiency of multiple mechanisms. The most common causes are thought to be immediate or delayed damage from childbirth, complications from prior anorectal surgery, altered bowel habits. An estimated 2.2% of community-dwelling adults are affected. However, reported prevalence figures vary. A prevalence of 8.39% among non-institutionalized U.S adults between 2005 and 2010 has been reported, and among institutionalized elders figures come close to 50%.

The levator ani is a broad, thin muscle group, situated on either side of the pelvis. It is formed from three muscle components: the pubococcygeus, the iliococcygeus, and the puborectalis.

Episiotomy, also known as perineotomy, is a surgical incision of the perineum and the posterior vaginal wall generally done by a midwife or obstetrician. Episiotomy is usually performed during second stage of labor to quickly enlarge the opening for the baby to pass through. The incision, which can be done from the posterior midline of the vulva straight toward the anus or at an angle to the right or left, is performed under local anesthetic, and is sutured after delivery.

A rectal prolapse occurs when walls of the rectum have prolapsed to such a degree that they protrude out of the anus and are visible outside the body. However, most researchers agree that there are 3 to 5 different types of rectal prolapse, depending on whether the prolapsed section is visible externally, and whether the full or only partial thickness of the rectal wall is involved.

The pelvic floor or pelvic diaphragm is a muscular partition separating the pelvic cavity (above), and perineal region (below). It is formed by the levator ani muscle and coccygeus muscle, and associated connective tissue.
In gynecology, a rectocele or posterior vaginal wall prolapse results when the rectum bulges (herniates) into the vagina. Two common causes of this defect are childbirth and hysterectomy. Rectocele also tends to occur with other forms of pelvic organ prolapse, such as enterocele, sigmoidocele and cystocele.

The external anal sphincter is a flat plane of skeletal muscle fibers, elliptical in shape and intimately adherent to the skin surrounding the margin of the anus.

The internal anal sphincter, IAS, is a ring of smooth muscle that surrounds about 2.5–4.0 cm of the anal canal; its inferior border is in contact with, but quite separate from, the external anal sphincter. It is myogenic in nature and playing phasic and tonic state for relaxation and contraction. This myogenic tone is based on Ca2+/Calmodulin/MLCK/RhoA/ROCK signaling cascade pathway. Recent studies suggested, BDNF is the member of the neurotrophin family; having next target for basal IAS and NANC relaxation.
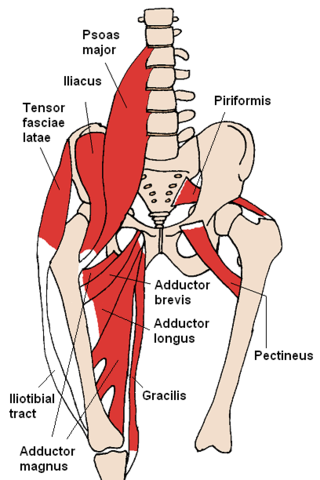
The gracilis muscle is the most superficial muscle on the medial side of the thigh. It is thin and flattened, broad above, narrow and tapering below.

Anal fistula is a chronic abnormal communication between the anal canal and usually the perianal skin. An anal fistula can be described as a narrow tunnel with its internal opening in the anal canal and its external opening in the skin near the anus. Anal fistulae commonly occur in people with a history of anal abscesses. They can form when anal abscesses do not heal properly.

The pelvic fasciae are the fascia of the pelvis and can be divided into:

Defecography is a type of medical radiological imaging in which the mechanics of a patient's defecation are visualized in real time using a fluoroscope. The anatomy and function of the anorectum and pelvic floor can be dynamically studied at various stages during defecation.

In humans, the anus is the external opening of the rectum, located inside the intergluteal cleft and separated from the genitals by the perineum. Two sphincters control the exit of feces from the body during an act of defecation, which is the primary function of the anus. These are the internal anal sphincter and the external anal sphincter, which are circular muscles that normally maintain constriction of the orifice and which relaxes as required by normal physiological functioning. The inner sphincter is involuntary and the outer is voluntary. It is located behind the perineum which is located behind the vagina or scrotum.

A perineal tear is a laceration of the skin and other soft tissue structures which, in women, separate the vagina from the anus. Perineal tears mainly occur in women as a result of vaginal childbirth, which strains the perineum. It is the most common form of obstetric injury. Tears vary widely in severity. The majority are superficial and may require no treatment, but severe tears can cause significant bleeding, long-term pain or dysfunction. A perineal tear is distinct from an episiotomy, in which the perineum is intentionally incised to facilitate delivery. Episiotomy, a very rapid birth, or large fetal size can lead to more severe tears which may require surgical intervention.
Obstructed defecation syndrome is a major cause of functional constipation, of which it is considered a subtype. It is characterized by difficult and/or incomplete emptying of the rectum with or without an actual reduction in the number of bowel movements per week. Normal definitions of functional constipation include infrequent bowel movements and hard stools. In contrast, ODS may occur with frequent bowel movements and even with soft stools, and the colonic transit time may be normal, but delayed in the rectum and sigmoid colon.
In fecal incontinence (FI), surgery may be carried out if conservative measures alone are not sufficient to control symptoms. There are many surgical options described for FI, and they can be considered in 4 general groups.
A rectovestibular fistula, also referred to simply as a vestibular fistula, is an anorectal congenital disorder where an abnormal connection (fistula) exists between the rectum and the vulval vestibule of the female genitalia.

The rectococcygeal muscles are two bands of smooth muscle tissue arising from the 2nd and 3rd coccygeal vertebrae, and passing downward and forward to blend with the rectal longitudinal smooth muscle fibers on the posterior wall of the anal canal.

The vaginal support structures are those muscles, bones, ligaments, tendons, membranes and fascia, of the pelvic floor that maintain the position of the vagina within the pelvic cavity and allow the normal functioning of the vagina and other reproductive structures in the female. Defects or injuries to these support structures in the pelvic floor leads to pelvic organ prolapse. Anatomical and congenital variations of vaginal support structures can predispose a woman to further dysfunction and prolapse later in life. The urethra is part of the anterior wall of the vagina and damage to the support structures there can lead to incontinence and urinary retention.
References
- ↑ Block, Irving; Rodriguez, Salvador (1975). "The Warren Operation for Anal Incontinence Caused by Disruption of the Anterior Segment of the Anal Sphincter, Perineal Body, and Rectovaginal Septum: Report of Five Cases". Diseases of the Colon and Rectum. 18 (1): 28–34. doi:10.1007/BF02587234. PMID 1126252. S2CID 35284019.