Related Research Articles

Carpal tunnel syndrome (CTS) is the collection of symptoms and signs associated with median neuropathy at the carpal tunnel. Most CTS is related to idiopathic compression of the median nerve as it travels through the wrist at the carpal tunnel (IMNCT). Idiopathic means that there is no other disease process contributing to pressure on the nerve. Most CTS is due to IMNCT. As with most structural issues, it occurs in both hands, and the strongest risk factor is genetics.

The radial nerve is a nerve in the human body that supplies the posterior portion of the upper limb. It innervates the medial and lateral heads of the triceps brachii muscle of the arm, as well as all 12 muscles in the posterior osteofascial compartment of the forearm and the associated joints and overlying skin.

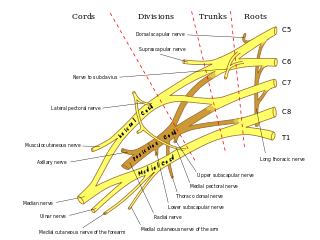
The median nerve is a nerve in humans and other animals in the upper limb. It is one of the five main nerves originating from the brachial plexus.
In human anatomy, the ulnar nerve is a nerve that runs near the ulna bone. The ulnar collateral ligament of elbow joint is in relation with the ulnar nerve. The nerve is the largest in the human body unprotected by muscle or bone, so injury is common. This nerve is directly connected to the little finger, and the adjacent half of the ring finger, innervating the palmar aspect of these fingers, including both front and back of the tips, perhaps as far back as the fingernail beds.

Wrist drop is a medical condition in which the wrist and the fingers cannot extend at the metacarpophalangeal joints. The wrist remains partially flexed due to an opposing action of flexor muscles of the forearm. As a result, the extensor muscles in the posterior compartment remain paralyzed.

The upper limbs or upper extremities are the forelimbs of an upright-postured tetrapod vertebrate, extending from the scapulae and clavicles down to and including the digits, including all the musculatures and ligaments involved with the shoulder, elbow, wrist and knuckle joints. In humans, each upper limb is divided into the arm, forearm and hand, and is primarily used for climbing, lifting and manipulating objects.
Myelopathy describes any neurologic deficit related to the spinal cord. When due to trauma, it is known as (acute) spinal cord injury. When inflammatory, it is known as myelitis. Disease that is vascular in nature is known as vascular myelopathy. The most common form of myelopathy in humans, cervical spondylotic myelopathy (CSM), is caused by arthritic changes (spondylosis) of the cervical spine, which result in narrowing of the spinal canal ultimately causing compression of the spinal cord. In Asian populations, spinal cord compression often occurs due to a different, inflammatory process affecting the posterior longitudinal ligament.

The opponens digiti minimi is a muscle in the hand. It is of a triangular form, and placed immediately beneath the palmaris brevis, abductor digiti minimi and flexor digiti minimi brevis. It is one of the three hypothenar muscles that control the little finger.

In human anatomy, the abductor digiti minimi is a skeletal muscle situated on the ulnar border of the palm of the hand. It forms the ulnar border of the palm and its spindle-like shape defines the hypothenar eminence of the palm together with the skin, connective tissue, and fat surrounding it. Its main function is to pull the little finger away from the other fingers.

The flexor digiti minimi brevis is a hypothenar muscle in the hand that flexes the little finger at the metacarpophalangeal joint. It lies lateral to the abductor digiti minimi when the hand is in anatomical position.

The anterior interosseous nerve is a branch of the median nerve that supplies the deep muscles on the anterior of the forearm, except the ulnar (medial) half of the flexor digitorum profundus. Its nerve roots come from C8 and T1.

Ulnar nerve entrapment is a condition where the ulnar nerve becomes physically trapped or pinched, resulting in pain, numbness, or weakness, primarily affecting the little finger and ring finger of the hand. Entrapment may occur at any point from the spine at cervical vertebra C7 to the wrist; the most common point of entrapment is in the elbow. Prevention is mostly through correct posture and avoiding repetitive or constant strain. Treatment is usually conservative, including medication, activity modification and exercise, but may sometimes include surgery. Prognosis is generally good, with mild to moderate symptoms often resolving spontaneously.

Ulnar neuropathy is a disorder involving the ulnar nerve. Ulnar neuropathy may be caused by entrapment of the ulnar nerve with resultant numbness and tingling. Motor function can be assessed by testing for a positive Froment's sign, or making an OK sign, little finger abduction can be tested as well.

The cervical spinal nerve 8 (C8) is a spinal nerve of the cervical segment.

An ulnar claw, also known as claw hand or 'spinster's claw', is a deformity or an abnormal attitude of the hand that develops due to ulnar nerve damage causing paralysis of the lumbricals. A claw hand presents with a hyperextension at the metacarpophalangeal joints and flexion at the proximal and distal interphalangeal joints of the 4th and 5th fingers. The patients with this condition can make a full fist but when they extend their fingers, the hand posture is referred to as claw hand. The ring- and little finger can usually not fully extend at the proximal interphalangeal joint (PIP).
The hand of benediction, also known as benediction sign or preacher's hand, occurs as a result of prolonged compression or injury of the median nerve at the forearm or elbow.

Pronator teres syndrome is a compression neuropathy of the median nerve at the elbow. It is rare compared to compression at the wrist or isolated injury of the anterior interosseous branch of the median nerve.

Injuries to the arm, forearm or wrist area can lead to various nerve disorders. One such disorder is median nerve palsy. The median nerve controls the majority of the muscles in the forearm. It controls abduction of the thumb, flexion of hand at wrist, flexion of digital phalanx of the fingers, is the sensory nerve for the first three fingers, etc. Because of this major role of the median nerve, it is also called the eye of the hand. If the median nerve is damaged, the ability to abduct and oppose the thumb may be lost due to paralysis of the thenar muscles. Various other symptoms can occur which may be repaired through surgery and tendon transfers. Tendon transfers have been very successful in restoring motor function and improving functional outcomes in patients with median nerve palsy.

Radial nerve dysfunction is a problem associated with the radial nerve resulting from injury consisting of acute trauma to the radial nerve. The damage has sensory consequences, as it interferes with the radial nerve's innervation of the skin of the posterior forearm, lateral three digits, and the dorsal surface of the lateral side of the palm. The damage also has motor consequences, as it interferes with the radial nerve's innervation of the muscles associated with the extension at the elbow, wrist, and fingers, as well the supination of the forearm. This type of injury can be difficult to localize, but relatively common, as many ordinary occurrences can lead to the injury and resulting mononeuropathy. One out of every ten patients suffering from radial nerve dysfunction do so because of a fractured humerus.

Monomelic amyotrophy (MMA) is a rare motor neuron disease first described in 1959 in Japan. Its symptoms usually appear about two years after adolescent growth spurt and is significantly more common in males, with an average age of onset between 15 and 25 years. MMA is reported most frequently in Asia but has a global distribution. It is typically marked by insidious onset of muscle atrophy of an upper limb, which plateaus after two to five years from which it neither improves nor worsens. There is no pain or sensory loss associated with MMA. MMA is not believed to be hereditary.
References
- ↑ Wilkinson, Iain and Lennox, Graham (June 2005). Essential Neurology (4th ed.). Wiley-Blackwell. p. 1184 ISBN 978-1-4051-1867-5.
- 1 2 Wartenberg, R. (1943-07-01). "Nerves of the Arm: Some of Their Affections; Their Diagnosis". California and Western Medicine. 59 (1): 22–24. ISSN 0093-4038. PMC 1780592 . PMID 18746534.
- ↑ Goldman, Sarah B.; Brininger, Teresa L.; Schrader, John W.; Koceja, David M. (2009-09-01). "A review of clinical tests and signs for the assessment of ulnar neuropathy". Journal of Hand Therapy. 22 (3): 209–219, quiz 220. doi:10.1016/j.jht.2008.10.010. ISSN 0894-1130. PMID 19188042.
- ↑ "Ulnar Neuropathy: Background, Anatomy, Pathophysiology".
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Posner, M. A. (2000-01-01). "Compressive neuropathies of the ulnar nerve at the elbow and wrist". Instructional Course Lectures. 49: 305–317. ISSN 0065-6895. PMID 10829185.
- ↑ Micev, Alan J.; Ivy, Andre D.; Aggarwal, Sandeep K.; Hsu, Wellington K.; Kalainov, David M. (2013-12-01). "Cervical radiculopathy and myelopathy: presentations in the hand". The Journal of Hand Surgery. 38 (12): 2478–2481, quiz 2481. doi:10.1016/j.jhsa.2013.07.020. ISSN 1531-6564. PMID 24054072.
- ↑ Ono, K.; Ebara, S.; Fuji, T.; Yonenobu, K.; Fujiwara, K.; Yamashita, K. (1987-03-01). "Myelopathy hand. New clinical signs of cervical cord damage". Bone & Joint Journal. 69-B (2): 215–219. ISSN 2049-4394. PMID 3818752.
- 1 2 Alter, M. (1973-05-01). "The digiti quinti sign of mild hemiparesis". Neurology. 23 (5): 503–505. doi:10.1212/wnl.23.5.503. ISSN 0028-3878. PMID 4735466.
- ↑ Vincent, M. B. (2009-05-01). "A Note on the Digiti Quinti Sign in Hemiplegic Migraine". Cephalalgia. 29 (5): 580–582. doi:10.1111/j.1468-2982.2008.01743.x. ISSN 0333-1024. PMID 19025551.
- ↑ Kuzuhara, Shigeki (2014-11-01). "[Robert Wartenberg: the neurologist, the teacher, and the man]". Brain and Nerve = Shinkei Kenkyū No Shinpo. 66 (11): 1301–1308. doi:10.11477/mf.1416200032. ISSN 1881-6096. PMID 25407064.