Emergency contraception (EC) is a birth control measure, used after sexual intercourse to prevent pregnancy.

The combined oral contraceptive pill (COCP), often referred to as the birth control pill or colloquially as "the pill", is a type of birth control that is designed to be taken orally by women. The pill contains two important hormones: a progestin and estrogen. When taken correctly, it alters the menstrual cycle to eliminate ovulation and prevent pregnancy.

Teenage pregnancy, also known as adolescent pregnancy, is thepregnancy of a female adolescent under the age of 20. This includes those who are legally considered adults in their country. The WHO defines adolescence as the period between the ages of 10 and 19 years. Pregnancy can occur with sexual intercourse after the start of ovulation, which can happen before the first menstrual period (menarche). In healthy, well-nourished girls, the first period usually takes place between the ages of 13 to 16.

Family planning is the consideration of the number of children a person wishes to have, including the choice to have no children, and the age at which they wish to have them. Things that may play a role on family planning decisions include marital situation, career or work considerations, financial situations. If sexually active, family planning may involve the use of contraception and other techniques to control the timing of reproduction.

Gillick competence is a term originating in England and Wales and is used in medical law to decide whether a child is able to consent to their own medical treatment, without the need for parental permission or knowledge.

Sexual health clinics specialize in the prevention and treatment of sexually transmitted infections.
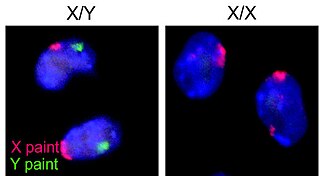
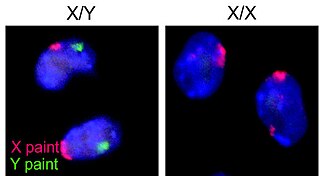
Human reproduction is sexual reproduction that results in human fertilization to produce a human offspring. It typically involves sexual intercourse between a sexually mature human male and female. During sexual intercourse, the interaction between the male and female reproductive systems results in fertilization of the ovum by the sperm to form a zygote. These specialized reproductive cells are called gametes, which are created in a process called gametogenesis. While normal cells contain 46 chromosomes, gamete cells only contain 23 single chromosomes, and it is when these two cells merge into one zygote cell that genetic recombination occurs and the new zygote contains 23 chromosomes from each parent, giving it 46 chromosomes. The zygote then undergoes a defined development process that is known as human embryogenesis, and this starts the typical 9-month gestation period that is followed by childbirth. The fertilization of the ovum may be achieved by artificial insemination methods, which do not involve sexual intercourse. Assisted reproductive technology also exists.

There are many methods of birth control that vary in requirements, side effects, and effectiveness. As the technology, education, and awareness about contraception has evolved, new contraception methods have been theorized and put in application. Although no method of birth control is ideal for every user, some methods remain more effective, affordable or intrusive than others. Outlined here are the different types of barrier methods, hormonal methods, various methods including spermicides, emergency contraceptives, and surgical methods and a comparison between them.
Adolescent sexuality is a stage of human development in which adolescents experience and explore sexual feelings. Interest in sexuality intensifies during the onset of puberty, and sexuality is often a vital aspect of teenagers' lives. Sexual interest may be expressed in a number of ways, such as flirting, kissing, masturbation, or having sex with a partner. Sexual interest among adolescents, as among adults, can vary greatly, and is influenced by cultural norms and mores, sex education, as well as comprehensive sexuality education provided, sexual orientation, and social controls such as age-of-consent laws.
The sexuality of US adolescents includes their feelings, behaviors and development, and the place adolescent sexuality has in American society, including the response of the government, educators, parents, and other interested groups.
Contraceptive security is an individual's ability to reliably choose, obtain, and use quality contraceptives for family planning and the prevention of sexually transmitted diseases. The term refers primarily to efforts undertaken in low and middle-income countries to ensure contraceptive availability as an integral part of family planning programs. Even though there is a consistent increase in the use of contraceptives in low, middle, and high-income countries, the actual contraceptive use varies in different regions of the world. The World Health Organization recognizes the importance of contraception and describes all choices regarding family planning as human rights. Subsidized products, particularly condoms and oral contraceptives, may be provided to increase accessibility for low-income people. Measures taken to provide contraceptive security may include strengthening contraceptive supply chains, forming contraceptive security committees, product quality assurance, promoting supportive policy environments, and examining financing options.

Birth control, also known as contraception, anticonception, and fertility control, is the use of methods or devices to prevent unintended pregnancy. Birth control has been used since ancient times, but effective and safe methods of birth control only became available in the 20th century. Planning, making available, and using human birth control is called family planning. Some cultures limit or discourage access to birth control because they consider it to be morally, religiously, or politically undesirable.

The birth control movement in the United States was a social reform campaign beginning in 1914 that aimed to increase the availability of contraception in the U.S. through education and legalization. The movement began in 1914 when a group of political radicals in New York City, led by Emma Goldman, Mary Dennett, and Margaret Sanger, became concerned about the hardships that childbirth and self-induced abortions brought to low-income women. Since contraception was considered to be obscene at the time, the activists targeted the Comstock laws, which prohibited distribution of any "obscene, lewd, and/or lascivious" materials through the mail. Hoping to provoke a favorable legal decision, Sanger deliberately broke the law by distributing The Woman Rebel, a newsletter containing a discussion of contraception. In 1916, Sanger opened the first birth control clinic in the United States, but the clinic was immediately shut down by police, and Sanger was sentenced to 30 days in jail.

Birth control in the United States is available in many forms. Some of the forms available at drugstores and some retail stores are male condoms, female condoms, sponges, spermicides, and over-the-counter emergency contraception. Forms available at pharmacies with a doctor's prescription or at doctor's offices are oral contraceptive pills, patches, vaginal rings, diaphragms, shots/injections, cervical caps, implantable rods, and intrauterine devices (IUDs). Sterilization procedures, including tubal ligations and vasectomies, are also performed.
The history of birth control, also known as contraception and fertility control, refers to the methods or devices that have been historically used to prevent pregnancy. Planning and provision of birth control is called family planning. In some times and cultures, abortion had none of the stigma which it has today, making birth control less important.
Adolescent sexuality in Canada is not as well documented as adolescent sexuality in the United States; despite the proximity of the two nations, Canada has its own unique culture and generalizations about Canadian adolescent sexuality based on American research can be misleading. Because of this, several surveys and studies have been conducted which acquired information on Canadian adolescent sexuality. Surveys which provide this information include the Canadian Community Health Survey (CCHS), the National Population Health Survey (NPHS) and the National Longitudinal Survey of Children and Youth (NLSCY). According to information drawn from the Canadian Community Health Survey and the National Population Health Survey, in 2005 43% of teens aged 15 to 19 reported that they had had sexual intercourse at least once.
Reproductive coercion is a collection of behaviors that interfere with decision-making related to reproductive health. These behaviors are meant to maintain power and control related to reproductive health by a current, former, or hopeful intimate or romantic partner, but they can also be perpetrated by parents or in-laws. Coercive behaviors infringe on individuals' reproductive rights and reduce their reproductive autonomy.

Access to safe and adequate sexual and reproductive healthcare constitutes part of the Universal Declaration of Human Rights, as upheld by the United Nations.
Contraceptive rights in New Zealand are extensive. There are many options available to women seeking contraception. There are also options for men. Government funding keeps the cost of most types of contraception low in most cases. Family planning options in New Zealand are generally in keeping with the United Nations stance towards sexual and reproductive rights although the country has received criticism in some aspects.

Margaret Ellen Mary O'Flynn, known professionally as Margaret Foley, was a British gynaecologist and pioneer of contraception services for women.