Rheumatoid arthritis (RA) is a long-term autoimmune disorder that primarily affects joints. It typically results in warm, swollen, and painful joints. Pain and stiffness often worsen following rest. Most commonly, the wrist and hands are involved, with the same joints typically involved on both sides of the body. The disease may also affect other parts of the body, including skin, eyes, lungs, heart, nerves, and blood. This may result in a low red blood cell count, inflammation around the lungs, and inflammation around the heart. Fever and low energy may also be present. Often, symptoms come on gradually over weeks to months.

Ankylosing spondylitis (AS) is a type of arthritis characterized by long-term inflammation of the joints of the spine, typically where the spine joins the pelvis. With AS, eye, bowel problems and back pain may occur. Joint mobility in the affected areas sometimes worsens over time. Ankylosing spondylitis is believed to involve a combination of genetic and environmental factors. More than 85% of people affected in the UK have a specific human leukocyte antigen known as the HLA-B27 antigen. The underlying mechanism is believed to be autoimmune or autoinflammatory. Diagnosis is based on symptoms with support from medical imaging and blood tests. AS is a type of seronegative spondyloarthropathy, meaning that tests show no presence of rheumatoid factor (RF) antibodies.

Disease-modifying antirheumatic drugs (DMARDs) comprise a category of otherwise unrelated disease-modifying drugs defined by their use in rheumatoid arthritis to slow down disease progression. The term is often used in contrast to nonsteroidal anti-inflammatory drugs and steroids.

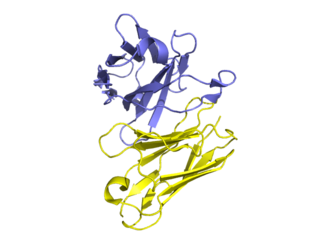
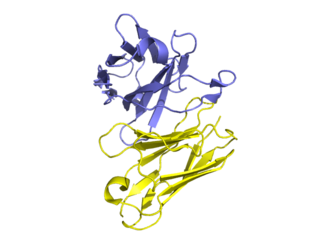
Human leukocyte antigen (HLA) B27 is a class I surface molecule encoded by the B locus in the major histocompatibility complex (MHC) on chromosome 6 and presents antigenic peptides to T cells. HLA-B27 is strongly associated with ankylosing spondylitis and other associated inflammatory diseases, such as psoriatic arthritis, inflammatory bowel disease, and reactive arthritis.
Spondyloarthropathy or spondyloarthrosis refers to any joint disease of the vertebral column. As such, it is a class or category of diseases rather than a single, specific entity. It differs from spondylopathy, which is a disease of the vertebra itself, but many conditions involve both spondylopathy and spondyloarthropathy.

Rheumatism or rheumatic disorders are conditions causing chronic, often intermittent pain affecting the joints or connective tissue. Rheumatism does not designate any specific disorder, but covers at least 200 different conditions, including arthritis and "non-articular rheumatism", also known as "regional pain syndrome" or "soft tissue rheumatism". There is a close overlap between the term soft tissue disorder and rheumatism. Sometimes the term "soft tissue rheumatic disorders" is used to describe these conditions.
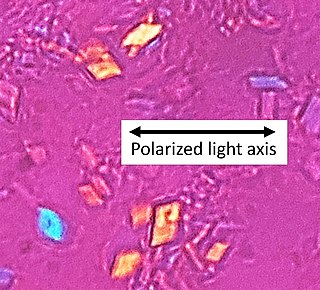
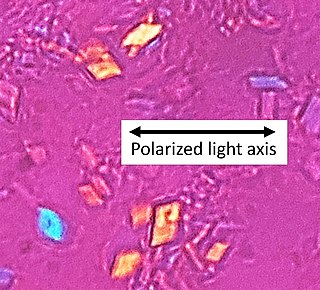
Calcium pyrophosphate dihydrate (CPPD) crystal deposition disease, also known as pseudogout and pyrophosphate arthropathy, is a rheumatologic disease which is thought to be secondary to abnormal accumulation of calcium pyrophosphate dihydrate crystals within joint soft tissues. The knee joint is most commonly affected. The disease is metabolic in origin and its treatment remains symptomatic.

Reactive arthritis, also known as Reiter's syndrome, is a form of inflammatory arthritis that develops in response to an infection in another part of the body (cross-reactivity). Coming into contact with bacteria and developing an infection can trigger the disease. By the time the patient presents with symptoms, often the "trigger" infection has been cured or is in remission in chronic cases, thus making determination of the initial cause difficult.
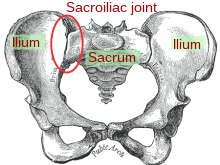
Sacroiliitis is inflammation within the sacroiliac joint. It is a feature of spondyloarthropathies, such as axial spondyloarthritis, psoriatic arthritis, reactive arthritis or arthritis related to inflammatory bowel diseases, including ulcerative colitis or Crohn's disease. It is also the most common presentation of arthritis from brucellosis.

Certolizumab pegol, sold under the brand name Cimzia, is a biopharmaceutical medication for the treatment of Crohn's disease, rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis. It is a fragment of a monoclonal antibody specific to tumor necrosis factor alpha (TNF-α) and is manufactured by UCB.
The BASDAI or Bath Ankylosing Spondylitis Disease Activity Index is a validated diagnostic test which allows a physician, usually a rheumatologist, to determine the effectiveness of a current drug therapy, or the need to institute a new drug therapy for the treatment of Ankylosing spondylitis (AS). The BASDAI is one of a group of classification criteria for spondyloarthropathies.
Biological response modifiers (BRMs) are substances that modify immune responses. They can be endogenous or exogenous, and they can either enhance an immune response or suppress it. Some of these substances arouse the body's response to an infection, and others can keep the response from becoming excessive. Thus they serve as immunomodulators in immunotherapy, which can be helpful in treating cancer and in treating autoimmune diseases, such as some kinds of arthritis and dermatitis. Most BRMs are biopharmaceuticals (biologics), including monoclonal antibodies, interleukin 2, interferons, and various types of colony-stimulating factors. "Immunotherapy makes use of BRMs to enhance the activity of the immune system to increase the body's natural defense mechanisms against cancer", whereas BRMs for rheumatoid arthritis aim to reduce inflammation.
Golimumab, sold under the brand name Simponi, is a human monoclonal antibody which is used as an immunosuppressive medication. Golimumab targets tumor necrosis factor alpha (TNF-alpha), a pro-inflammatory molecule and hence is a TNF inhibitor. Profound reduction in C-reactive protein (CRP) levels, interleukin (IL)-6, intercellaular adhesion molecules (ICAM)-1, matrix metalloproteinase (MMP)-3, and vascular endothelial growth factor (VEGF) demonstrates golimumab as an effective modulator of inflammatory markers and bone metabolism. Golimumab is given via subcutaneous injection.

Enteropathic arthropathy commonly referred to as enteropathic arthritis, is a type of arthritis linked to Crohn's disease, ulcerative colitis, and chronic inflammatory bowel diseases.

Secukinumab, sold under the brand name Cosentyx among others, is a human IgG1κ monoclonal antibody used for the treatment of psoriasis, ankylosing spondylitis, and psoriatic arthritis. It binds to the protein interleukin (IL)-17A and is marketed by Novartis.
Sarilumab, sold under the brand name Kevzara, is a human monoclonal antibody medication against the interleukin-6 receptor. Regeneron Pharmaceuticals and Sanofi developed the drug for the treatment of rheumatoid arthritis (RA), for which it received US FDA approval on 22 May 2017 and European Medicines Agency approval on 23 June 2017.
The Ankylosing Spondylitis Quality of Life (ASQoL) questionnaire is a patient-reported outcome (PRO) measure which assesses the quality of life of patients with ankylosing spondylitis. The ASQoL is based on the needs-based quality of life model. It is a self-administered questionnaire which contains 18 items and takes up to four minutes to complete.
Interleukin-38 (IL-38) is a member of the interleukin-1 (IL-1) family and the interleukin-36 (IL-36) subfamily. It is important for the inflammation and host defense. This cytokine is named IL-1F10 in humans and has similar three dimensional structure as IL-1 receptor antagonist (IL-1Ra). The organisation of IL-1F10 gene is conserved with other members of IL-1 family within chromosome 2q13. IL-38 is produced by mammalian cells may bind the IL-1 receptor type I. It is expressed in basal epithelia of skin, in proliferating B cells of the tonsil, in spleen and other tissues. This cytokine is playing important role in regulation of innate and adaptive immunity.
In radiology, a Romanus lesion is the erosion of the anterior and posterior vertebral endplates in patients with an inflammatory spondyloarthropathy – such as ankylosing spondylitis or an enteropathic arthropathy. The anterior erosion in particular causes a loss of anterior vertebral body concavity, causing the vertebra to display a squared contour or even a barrel-shape. Healing of the erosion results in a sclerotic increase in density causing what is known as a shiny corner sign, which can later result in syndesmophyte formation. It is most easily diagnosed using MRI, compared to conventional radiography.
Diagnostic delay is the time interval between the onset of symptoms and confirmed diagnosis of a disease. For a variety of reasons, including the mitigation of disease severity and financial expense, it is desirable for this delay to be minimized.