Related Research Articles

Alcoholism is, broadly, any drinking of alcohol that results in significant mental or physical health problems. Because there is disagreement on the definition of the word alcoholism, it is not a recognized diagnostic entity, and the use of alcoholism terminology is discouraged due to its heavily stigmatized connotations. Predominant diagnostic classifications are alcohol use disorder (DSM-5) or alcohol dependence (ICD-11); these are defined in their respective sources.

Alcohol intoxication, also known in overdose as alcohol poisoning, commonly described as drunkenness or inebriation, is the behavior and physical effects caused by a recent consumption of alcohol. In addition to the toxicity of ethanol, the main psychoactive component of alcoholic beverages, other physiological symptoms may arise from the activity of acetaldehyde, a metabolite of alcohol. These effects may not arise until hours after ingestion and may contribute to the condition colloquially known as a hangover.

Alcohol abuse encompasses a spectrum of unhealthy alcohol drinking behaviors, ranging from binge drinking to alcohol dependence, in extreme cases resulting in health problems for individuals and large scale social problems such as alcohol-related crimes.
The long-term heavy consumption of alcohol can cause severe detrimental effects. Health effects associated with alcohol intake in large amounts include an increased risk of developing an alcohol use disorder, malnutrition, chronic pancreatitis, erectile dysfunction, heart failure, atrial fibrillation, gastritis, stomach ulcers, alcoholic liver disease, certain types of dementia, and several types of cancer. In addition, damage to the central nervous system and peripheral nervous system can occur from chronic heavy alcohol consumption. There is also an increased risk for accidental injuries, for example, those sustained in traffic accidents and falls. Studies show that individuals with heavy substance use have a much higher risk of having other disorders. A cross-sectional observational study found evidence that people who used substances had the highest risk for five of the disorders studied. However, even light and moderate alcohol consumption increase the risk for developing certain types of cancer. Among women, light drinkers have a four percent increase risk of breast cancer, while moderate drinkers have a 23 percent increase in risk of the disease.
Alcohol education is the practice of disseminating information about the effects of alcohol on health, as well as society and the family unit. It was introduced into the public schools by temperance organizations such as the Woman's Christian Temperance Union in the late 19th century. Initially, alcohol education focused on how the consumption of alcoholic beverages affected society, as well as the family unit. In the 1930s, this came to also incorporate education pertaining to alcohol's effects on health. For example, even light and moderate alcohol consumption increases cancer risk in individuals. Organizations such as the National Institute on Alcohol Abuse and Alcoholism in the United States were founded to promulgate alcohol education alongside those of the temperance movement, such as the American Council on Alcohol Problems.
Alcohol has a number of effects on health. Short-term effects of alcohol consumption include intoxication and dehydration. Long-term effects of alcohol include changes in the metabolism of the liver and brain, several types of cancer and alcohol use disorder. Alcohol intoxication affects the brain, causing slurred speech, clumsiness, and delayed reflexes. Alcohol consumption can cause hypoglycemia in diabetics on certain medications, such as insulin or sulfonylurea, by blocking gluconeogenesis. There is an increased risk of developing an alcohol use disorder for teenagers while their brain is still developing. Adolescents who drink have a higher probability of injury including death.
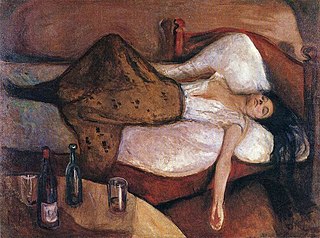
A hangover is the experience of various unpleasant physiological and psychological effects usually following the consumption of alcohol, such as wine, beer, and liquor. Hangovers can last for several hours or for more than 24 hours. Typical symptoms of a hangover may include headache, drowsiness, concentration problems, dry mouth, dizziness, fatigue, gastrointestinal distress, absence of hunger, light sensitivity, depression, sweating, nausea, hyper-excitability, irritability, and anxiety.

The short-term effects of alcohol consumption range from a decrease in anxiety and motor skills and euphoria at lower doses to intoxication (drunkenness), to stupor, unconsciousness, anterograde amnesia, and central nervous system depression at higher doses. Cell membranes are highly permeable to alcohol, so once alcohol is in the bloodstream, it can diffuse into nearly every cell in the body.

Binge drinking, or heavy episodic drinking, is drinking alcoholic beverages with an intention of becoming intoxicated by heavy consumption of alcohol over a short period of time, but definitions vary considerably.
Alcohol and sex deals with the effects of the consumption of alcohol on sexual behavior. The effects of alcohol are balanced between its suppressive effects on sexual physiology, which will decrease sexual activity, and its suppression of psychological inhibitions, which may increase the desire for sex.

Ethanol is the type of alcohol found in alcoholic beverages. It is a volatile, flammable, colorless liquid that acts as a central nervous system depressant. Ethanol can impair different types of memory.
Kindling due to substance withdrawal refers to the neurological condition which results from repeated withdrawal episodes from sedative–hypnotic drugs such as alcohol and benzodiazepines.

A caffeinated alcoholic drink is a drink that contains both alcohol and a significant amount of caffeine. Caffeine, a stimulant, masks some of the depressant effects of alcohol. However, in 2010 and 2011, this type of drink faced criticism for posing health risks to its drinkers. In some places there is a ban on caffeinated alcoholic drinks.
Recent research has looked into the effects of alcohol on the amount of cortisol that is produced in the human body. Continuous consumption of alcohol over an extended period of time has been shown to raise cortisol levels in the body. Cortisol is released during periods of high stress, and can result in the temporary shut down of other physical processes, causing physical damage to the body.
Drunkorexia is a colloquialism for anorexia or bulimia combined with an alcohol use disorder. The term is generally used to denote the utilization of extreme weight control methods to compensate for planned binge drinking. Research on the combination of an eating disorder and binge drinking has primarily focused on college-aged women, though the phenomenon has also been noted among young men. Studies suggest that individuals engage in this combination of self-imposed malnutrition and binge drinking to avoid weight gain from alcohol, to save money for purchasing alcohol, and to facilitate alcohol intoxication.
While researchers have found that moderate alcohol consumption in older adults is associated with better cognition and well-being than abstinence, excessive alcohol consumption is associated with widespread and significant brain lesions. Other data – including investigated brain-scans of 36,678 UK Biobank participants – suggest that even "light" or "moderate" consumption of alcohol by itself harms the brain, such as by reducing brain grey matter volume. This may imply that alternatives and generally aiming for lowest possible consumption could usually be the advisable approach.

Alcohol, sometimes referred to by the chemical name ethanol, is a depressant drug that is the active ingredient in drinks such as beer, wine, and distilled spirits. It is one of the oldest and most commonly consumed recreational drugs, causing the characteristic effects of alcohol intoxication ("drunkenness"). Among other effects, alcohol produces happiness and euphoria, decreased anxiety, increased sociability, sedation, impairment of cognitive, memory, motor, and sensory function, and generalized depression of central nervous system (CNS) function. Ethanol is only one of several types of alcohol, but it is the only type of alcohol that is found in alcoholic beverages or commonly used for recreational purposes; other alcohols such as methanol and isopropyl alcohol are significantly more toxic. A mild, brief exposure to isopropanol, being only moderately more toxic than ethanol, is unlikely to cause any serious harm. Methanol, being profoundly more toxic than ethanol, is lethal in quantities as small as 10–15 milliliters.
Alcohol-related brain damage alters both the structure and function of the brain as a result of the direct neurotoxic effects of alcohol intoxication or acute alcohol withdrawal. Increased alcohol intake is associated with damage to brain regions including the frontal lobe, limbic system, and cerebellum, with widespread cerebral atrophy, or brain shrinkage caused by neuron degeneration. This damage can be seen on neuroimaging scans.
Subjective response to alcohol (SR) refers to an individual's unique experience of the pharmacological effects of alcohol and is a putative risk factor for the development of alcoholism. Subjective effects include both stimulating experiences typically occurring during the beginning of a drinking episode as breath alcohol content (BAC) rises and sedative effects, which are more prevalent later in a drinking episode as BAC wanes. The combined influence of hedonic and aversive subjective experiences over the course of a drinking session are strong predictors of alcohol consumption and drinking consequences. There is also mounting evidence for consideration of SR as an endophenotype with some studies suggesting that it accounts for a significant proportion of genetic risk for the development of alcohol use disorder.
Many students attending colleges, universities, and other higher education institutions consume alcoholic beverages. The laws and social culture around this practice vary by country and institution type, and within an institution, some students may drink heavily whereas others may not drink at all. In the United States, drinking tends to be particularly associated with fraternities.
References
- ↑ Melchior, C (1996). "Neurosteroids block the memory-impairing effects of ethanol in mice". Pharmacology Biochemistry and Behavior. 53 (1): 51–6. doi:10.1016/0091-3057(95)00197-2. PMID 8848460. S2CID 30580813.
- ↑ Marsh, Beth; Carlyle, Molly; Carter, Emily; Hughes, Paige; McGahey, Sarah; Lawn, Will; Stevens, Tobias; McAndrew, Amy; Morgan, Celia J. A. (2019-03-01). "Shyness, alcohol use disorders and 'hangxiety': A naturalistic study of social drinkers". Personality and Individual Differences. 139: 13–18. doi:10.1016/j.paid.2018.10.034. hdl: 10871/34832 . ISSN 0191-8869. S2CID 149543533.
- ↑ "Blackout".
- ↑ Parker, Elizabeth S; Birnbaum, Isabel M; Noble, Ernest P (1976). "Alcohol and memory: Storage and state dependency". Journal of Verbal Learning and Verbal Behavior. 15 (6): 691–702. doi:10.1016/0022-5371(76)90061-X.
- ↑ Acheson, Shawn K; Stein, Roy M; Swartzwelder, H. S (1998). "Impairment of Semantic and Figural Memory by Acute Ethanol: Age-Dependent Effects". Alcoholism: Clinical and Experimental Research. 22 (7): 1437–42. doi:10.1111/j.1530-0277.1998.tb03932.x. PMID 9802525.
- ↑ White, Aaron M; Jamieson-Drake, David W; Swartzwelder, H Scott (2002). "Prevalence and Correlates of Alcohol-Induced Blackouts Among College Students: Results of an E-Mail Survey". Journal of American College Health. 51 (3): 117–9, 122–31. doi:10.1080/07448480209596339. PMID 12638993. S2CID 24467307 . Retrieved February 12, 2003.
- ↑ Wetherill, Reagan R; Fromme, Kim (2011). "Acute alcohol effects on narrative recall and contextual memory: An examination of fragmentary blackouts". Addictive Behaviors. 36 (8): 886–9. doi:10.1016/j.addbeh.2011.03.012. PMC 3101897 . PMID 21497445.
- ↑ Wetherill, Reagan R; Schnyer, David M; Fromme, Kim (2012). "Acute Alcohol Effects on Contextual Memory BOLD Response: Differences Based on Fragmentary Blackout History". Alcoholism: Clinical and Experimental Research. 36 (6): 1108–15. doi:10.1111/j.1530-0277.2011.01702.x. PMC 3370058 . PMID 22420742.
- 1 2 Goodwin, Donald W; Crane, J Bruce; Guze, Samuel B (1969). "Alcoholic "Blackouts": A Review and Clinical Study of 100 Alcoholics". American Journal of Psychiatry. 126 (2): 191–8. doi:10.1176/ajp.126.2.191. PMID 5804804.
- ↑ White, Aaron M; Signer, Matthew L; Kraus, Courtney L; Swartzwelder, H Scott (2009). "Experiential Aspects of Alcohol‐Induced Blackouts Among College Students". The American Journal of Drug and Alcohol Abuse. 30 (1): 205–24. doi:10.1081/ADA-120029874. PMID 15083562. S2CID 9925229.
- ↑ Lee, Hamin; Roh, Sungwon; Kim, Dai Jin (2009). "Alcohol-Induced Blackout". International Journal of Environmental Research and Public Health. 6 (11): 2783–92. doi: 10.3390/ijerph6112783 . PMC 2800062 . PMID 20049223.
- ↑ Ryback, R. S (1970). "Alcohol amnesia. Observations in seven drinking inpatient alcoholics". Quarterly Journal of Studies on Alcohol. 31 (3): 616–32. doi:10.15288/qjsa.1970.31.616. PMID 5458472.
- ↑ o'Mahony, John F (2004). "A Comparison of Alcohol Abusers Who Have and Have Not Experienced Blackouts" (PDF). European Addiction Research. 10 (3): 95–8. doi:10.1159/000077696. PMID 15258438. S2CID 11767192.
- ↑ Wetherill, Reagan R; Fromme, Kim (2009). "Subjective Responses to Alcohol Prime Event-Specific Alcohol Consumption and Predict Blackouts and Hangover". Journal of Studies on Alcohol and Drugs. 70 (4): 593–600. doi:10.15288/jsad.2009.70.593. PMC 2696300 . PMID 19515300.
- ↑ Perry, Paul J; Argo, Tami R; Barnett, Mitchell J; Liesveld, Jill L; Liskow, Barry; Hernan, Jillian M; Trnka, Michael G; Brabson, Mary A (2006). "The Association of Alcohol-Induced Blackouts and Grayouts to Blood Alcohol Concentrations". Journal of Forensic Sciences. 51 (4): 896–9. doi:10.1111/j.1556-4029.2006.00161.x. PMID 16882236. S2CID 22730363.
- ↑ Wetherill, Reagan R; Castro, Norma; Squeglia, Lindsay M; Tapert, Susan F (2013). "Atypical neural activity during inhibitory processing in substance-naïve youth who later experience alcohol-induced blackouts". Drug and Alcohol Dependence. 128 (3): 243–9. doi:10.1016/j.drugalcdep.2012.09.003. PMC 3552086 . PMID 23021773.
- ↑ Hartzler, Bryan; Fromme, Kim (2003). "Fragmentary and en bloc blackouts: Similarity and distinction among episodes of alcohol-induced memory loss". Journal of Studies on Alcohol. 64 (4): 547–50. doi:10.15288/jsa.2003.64.547. PMID 12921196. S2CID 25840438.
- ↑ Baer, John S; Sampson, Paul D; Barr, Helen M; Connor, Paul D; Streissguth, Ann P (2003). "A 21-Year Longitudinal Analysis of the Effects of Prenatal Alcohol Exposure on Young Adult Drinking". Archives of General Psychiatry. 60 (4): 377–85. doi: 10.1001/archpsyc.60.4.377 . PMID 12695315.
- ↑ Nelson, Elliot C; Heath, Andrew C; Bucholz, Kathleen K; Madden, Pamela A. F; Fu, Qiang; Knopik, Valerie; Lynskey, Michael T; Whitfield, John B; Statham, Dixie J; Martin, Nicholas G (2004). "Genetic Epidemiology of Alcohol-Induced Blackouts". Archives of General Psychiatry. 61 (3): 257–63. doi: 10.1001/archpsyc.61.3.257 . PMID 14993113.
- ↑ Davis, Christal; Slutske, Wendy; Martin, Nicholas; Agrawal, Arpana; Lynskey, Michael (2019). "Genetic Epidemiology of Liability for Alcohol-Induced Blacking and Passing Out". Alcoholism: Clinical and Experimental Research. 43 (6): 1103–1112. doi:10.1111/acer.14045. PMC 6551280 . PMID 31063677.
- ↑ Vignau, J; Soichot, M; Imbenotte, M; Jacquemont, M.-C; Danel, T; Vandamme, M; Lhermitte, M; Allorge, D (2009). "Impact of Tryptophan Metabolism on the Vulnerability to Alcohol-Related Blackouts and Violent Impulsive Behaviours". Alcohol and Alcoholism. 45 (1): 79–88. doi: 10.1093/alcalc/agp044 . PMID 19759277.
- ↑ Buelow, G.; Harbin, J. (Fall 1996). "The Influence of Blackouts on Alcohol Use Expectancies". Journal of Alcohol and Drug Education. 42 (1): 25. Retrieved October 8, 2012.
- ↑ Buelow, G.; Koeppel, J. (1995). "Psychological Consequences of Alcohol Induced Blackouts among college students". Journal of Alcohol and Drug Education. 40 (3): 10–20. Retrieved October 8, 2012.
- ↑ Van Oorsouw, K; Merckelbach, H; Ravelli, D; Nijman, H; Mekking-Pompen, I (2004). "Alcoholic blackout for criminally relevant behavior". The Journal of the American Academy of Psychiatry and the Law. 32 (4): 364–70. PMID 15704619.
- ↑ Wray, Tyler B; Simons, Jeffrey S; Dvorak, Robert D; Gaher, Raluca M (2012). "Trait-based affective processes in alcohol-involved "risk behaviors"". Addictive Behaviors. 37 (11): 1230–9. doi:10.1016/j.addbeh.2012.06.004. PMC 3401606 . PMID 22770825.