Related Research Articles

The United States Food and Drug Administration is a federal agency of the Department of Health and Human Services. The FDA is responsible for protecting and promoting public health through the control and supervision of food safety, tobacco products, caffeine products, dietary supplements, prescription and over-the-counter pharmaceutical drugs (medications), vaccines, biopharmaceuticals, blood transfusions, medical devices, electromagnetic radiation emitting devices (ERED), cosmetics, animal foods & feed and veterinary products.
Health Canada is the department of the Government of Canada responsible for national health policy. The department itself is also responsible for numerous federal health-related agencies, including the Canadian Food Inspection Agency (CFIA) and the Public Health Agency of Canada (PHAC), among others. These organizations help to ensure compliance with federal law in a variety of healthcare, agricultural, and pharmaceutical activities. This responsibility also involves extensive collaboration with various other federal- and provincial-level organizations in order to ensure the safety of food, health, and pharmaceutical products—including the regulation of health research and pharmaceutical manufacturing/testing facilities.
The regulation of science refers to use of law, or other ruling, by academic or governmental bodies to allow or restrict science from performing certain practices, or researching certain scientific areas.
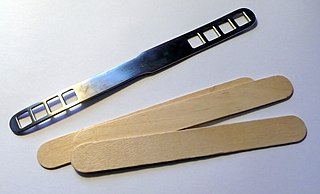
A medical device is any device intended to be used for medical purposes. Significant potential for hazards are inherent when using a device for medical purposes and thus medical devices must be proved safe and effective with reasonable assurance before regulating governments allow marketing of the device in their country. As a general rule, as the associated risk of the device increases the amount of testing required to establish safety and efficacy also increases. Further, as associated risk increases the potential benefit to the patient must also increase.

The Biologics Control Act of 1902, also known as the Virus-Toxin Law, was the first law that implemented federal regulations of biological products such as vaccines in the United States. It was enacted in response to two incidents involving the deaths of 22 children who had contracted tetanus from contaminated vaccines. This law paved the way for further regulation of drug products under the Pure Food and Drug Act of 1906 and the Federal Food, Drug, and Cosmetic Act of 1938. Biologics control is now under the supervision of the U.S. Food and Drug Administration (FDA).
Title 21 is the portion of the Code of Federal Regulations that governs food and drugs within the United States for the Food and Drug Administration (FDA), the Drug Enforcement Administration (DEA), and the Office of National Drug Control Policy (ONDCP).

The Center for Drug Evaluation and Research is a division of the U.S. Food and Drug Administration (FDA) that monitors most drugs as defined in the Food, Drug, and Cosmetic Act. Some biological products are also legally considered drugs, but they are covered by the Center for Biologics Evaluation and Research. The center reviews applications for brand name, generic, and over the counter pharmaceuticals, manages US current Good Manufacturing Practice (cGMP) regulations for pharmaceutical manufacturing, determines which medications require a medical prescription, monitors advertising of approved medications, and collects and analyzes safety data about pharmaceuticals that are already on the market.

The Center for Devices and Radiological Health (CDRH) is the branch of the United States Food and Drug Administration (FDA) responsible for the premarket approval of all medical devices, as well as overseeing the manufacturing, performance and safety of these devices. The CDRH also oversees the radiation safety performance of non-medical devices which emit certain types of electromagnetic radiation, such as cellular phones and microwave ovens.
Numerous governmental and non-governmental organizations have criticized the U. S. Food and Drug Administration for alleged excessive and/or insufficient regulation. The U.S. Food and Drug Administration (FDA) is an agency of the United States Department of Health and Human Services and is responsible for the safety regulation of most types of foods, dietary supplements, drugs, vaccines, biological medical products, blood products, medical devices, radiation-emitting devices, veterinary products, and cosmetics. The FDA also enforces section 361 of the Public Health Service Act and the associated regulations, including sanitation requirements on interstate travel as well as specific rules for control of disease on products ranging from animals sold as pets to donations of human blood and tissue.
Good clinical data management practice (GCDMP) is the current industry standards for clinical data management that consist of best business practice and acceptable regulatory standards. In all phases of clinical trials, clinical and laboratory information must be collected and converted to digital form for analysis and reporting purposes. The U.S. Food and Drug Administration and International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use have provided specific regulations and guidelines surrounding this component of the drug and device development process. The effective, efficient and regulatory-compliant management of clinical trial data is an essential component of drug and device development.
Good tissue practice (GTP) is one of the "GxP" requirements derived from good manufacturing practice. The rule was written and is enforced by the U.S. Food and Drug Administration (FDA), specifically the Center for Biologics Evaluation and Research. The authority for the regulation comes from the Public Health Service Act and all of the requirements relate to transmission of communicable disease, including bacterial or fungal contamination during processing.

President of the United States George W. Bush signed the Food and Drug Administration Amendments Act of 2007 (FDAAA) on September 27, 2007. This law reviewed, expanded, and reaffirmed several existing pieces of legislation regulating the FDA. These changes allow the FDA to perform more comprehensive reviews of potential new drugs and devices. It was sponsored by Reps. Joe Barton and Frank Pallone and passed unanimously by the Senate.
The following outline is provided as an overview of and topical guide to clinical research:
An Emergency Use Authorization (EUA) in the United States is an authorization granted to the Food and Drug Administration (FDA) under sections of the Federal Food, Drug, and Cosmetic Act as added to and amended by various Acts of Congress, including by the Pandemic and All-Hazards Preparedness Reauthorization Act of 2013 (PAHPRA), as codified by 21 U.S.C. § 360bbb-3, to allow the use of a drug prior to approval. It does not constitute approval of the drug in the full statutory meaning of the term, but instead authorizes the FDA to facilitate availability of an unapproved product, or an unapproved use of an approved product, during a declared state of emergency from one of several agencies or of a "material threat" by the Secretary of Homeland Security.
The FDA animal efficacy rule applies to development and testing of drugs and biologicals to reduce or prevent serious or life-threatening conditions caused by exposure to lethal or permanently disabling toxic agents, where human efficacy trials are not feasible or ethical. The animal efficacy rule was finalized by the FDA and authorized by the United States Congress in 2002, following the September 11 attacks and concerns regarding bioterrorism.
An FDA warning letter is an official message from the United States Food and Drug Administration (FDA) to a manufacturer or other organization that has violated some rule in a federally regulated activity.
A biologics license application (BLA) is defined by the U.S. Food and Drug Administration (FDA) as follows:
The FDA Adverse Event Reporting System is a computerized information database designed to support the U.S. Food and Drug Administration's (FDA) postmarketing safety surveillance program for all approved drug and therapeutic biologic products. The FDA uses FAERS to monitor for new adverse events and medication errors that might occur with these products. It is a system that measures occasional harms from medications to ascertain whether the risk–benefit ratio is high enough to justify continued use of any particular drug and to identify correctable and preventable problems in health care delivery. The system interacts with several related systems including MedWatch and the Vaccine Adverse Event Reporting System. FAERS replaced legacy AERS system in Sep 2012.
Breakthrough therapy is a United States Food and Drug Administration designation that expedites drug development that was created by Congress under Section 902 of the 9 July 2012 Food and Drug Administration Safety and Innovation Act. The FDA's "breakthrough therapy" designation is not intended to imply that a drug is actually a "breakthrough" or that there is high-quality evidence of treatment efficacy for a particular condition; rather, it allows the FDA to grant priority review to drug candidates if preliminary clinical trials indicate that the therapy may offer substantial treatment advantages over existing options for patients with serious or life-threatening diseases. The FDA has other mechanisms for expediting the review and approval process for promising drugs, including fast track designation, accelerated approval, and priority review.

Janet Woodcock is an American physician and former Acting Commissioner of the U.S. Food and Drug Administration (FDA). She joined the FDA in 1986, and has held a number of senior leadership positions there, including terms as the Director of Center for Drug Evaluation and Research (CDER) from 1994 to 2004 and 2007 to 2021.
References
- ↑ McDonald, Sharon. (September 2002) "Science and the Regulation of Biological Products: From a Rich History to a Challenging Future." Center for Biologics Evaluation and Research.
- ↑ "Director, Office of Blood Research and Review (OBRR)". About the Center for Biologics Evaluation and Research (Job posting). FDA. 28 March 2018. Retrieved 28 March 2018.[ self-published source ]
- ↑ CBER website, About CBER Retrieved August 30, 2012.
- ↑ "Keeping the public healthy". KM World. October 2003.
- ↑ "Transcript of U.S. FDA Center for Biologics Evaluation and Research Vaccines and Related Biological Products Advisory Committee's 101st meeting of February 16, 2005". origin.www.fda.gov. Archived from the original (DOC) on 2009-09-01.
- ↑ "in Google provided HTML format".
- ↑ Kim Coghill (16 December 2002). "ZOON RESIGNS POSITION AT CBER, PLANS MOVE TO CANCER INSTITUTE". BIOWORLD Today.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Reid, Ken. "CBER and CDER have long history of being lumped together and split up." Bioresearch Monitoring Alert Sept. 2002. page 4.
- ↑ "Advisory Committee Laws, Regulations and Guidance". Food and Drug Administration. 27 March 2018. Retrieved 20 December 2020.
- ↑ "Committees and Meeting Materials". Food and Drug Administration. 29 November 2018. Retrieved 20 December 2020.