Back pain is pain felt in the back. It may be classified as neck pain (cervical), middle back pain (thoracic), lower back pain (lumbar) or coccydynia based on the segment affected. The lumbar area is the most common area affected. An episode of back pain may be acute, subacute or chronic depending on the duration. The pain may be characterized as a dull ache, shooting or piercing pain or a burning sensation. Discomfort can radiate to the arms and hands as well as the legs or feet, and may include numbness or weakness in the legs and arms.

Back injuries result from damage, wear, or trauma to the bones, muscles, or other tissues of the back. Common back injuries include sprains and strains, herniated discs, and fractured vertebrae. The lumbar spine is often the site of back pain. The area is susceptible because of its flexibility and the amount of body weight it regularly bears. It is estimated that low-back pain may affect as much as 80 to 90 percent of the general population in the United States.

Spondylosis is the degeneration of the vertebral column from any cause. In the more narrow sense it refers to spinal osteoarthritis, the age-related degeneration of the spinal column, which is the most common cause of spondylosis. The degenerative process in osteoarthritis chiefly affects the vertebral bodies, the neural foramina and the facet joints. If severe, it may cause pressure on the spinal cord or nerve roots with subsequent sensory or motor disturbances, such as pain, paresthesia, imbalance, and muscle weakness in the limbs.

A spinal cord injury (SCI) is damage to the spinal cord that causes temporary or permanent changes in its function. Symptoms may include loss of muscle function, sensation, or autonomic function in the parts of the body served by the spinal cord below the level of the injury. Injury can occur at any level of the spinal cord and can be complete, with a total loss of sensation and muscle function at lower sacral segments, or incomplete, meaning some nervous signals are able to travel past the injured area of the cord up to the Sacral S4-5 spinal cord segments. Depending on the location and severity of damage, the symptoms vary, from numbness to paralysis, including bowel or bladder incontinence. Long term outcomes also range widely, from full recovery to permanent tetraplegia or paraplegia. Complications can include muscle atrophy, loss of voluntary motor control, spasticity, pressure sores, infections, and breathing problems.

A cervical collar, also known as a neck brace, is a medical device used to support and immobilize a person's neck. It is also applied by emergency personnel to those who have had traumatic head or neck injuries, and can be used to treat chronic medical conditions.

A cervical fracture, commonly called a broken neck, is a fracture of any of the seven cervical vertebrae in the neck. Examples of common causes in humans are traffic collisions and diving into shallow water. Abnormal movement of neck bones or pieces of bone can cause a spinal cord injury, resulting in loss of sensation, paralysis, or usually death soon thereafter, primarily via compromising neurological supply to the respiratory muscles as well as innervation to the heart.

Spondylolisthesis is the displacement of one spinal vertebra compared to another. While some medical dictionaries define spondylolisthesis specifically as the forward or anterior displacement of a vertebra over the vertebra inferior to it, it is often defined in medical textbooks as displacement in any direction. Spondylolisthesis is graded based upon the degree of slippage of one vertebral body relative to the subsequent adjacent vertebral body. Spondylolisthesis is classified as one of the six major etiologies: degenerative, traumatic, dysplastic, isthmic, pathologic, or post-surgical. Spondylolisthesis most commonly occurs in the lumbar spine, primarily at the L5-S1 level, with the L5 vertebral body anteriorly translating over the S1 vertebral body.
A skeletal survey is a series of X-rays of all the bones in the body, or at least the axial skeleton and the large cortical bones. A very common use is the diagnosis of multiple myeloma, where tumour deposits appear as "punched-out" lesions. The standard set of X-rays for a skeletal survey includes X-rays of the skull, entire spine, pelvis, ribs, both humeri and femora. It is more effective than isotope scans at detecting bone involvement in multiple myeloma. Although significantly less sensitive than MRI, it is easier to include more bones. A study found that MRI of just the spine and pelvis would have detected 9% fewer cases of bone involvement than the more extensive skeletal survey which therefore remains the standard method.
A burst fracture is a type of traumatic spinal injury in which a vertebra breaks from a high-energy axial load, with shards of vertebra penetrating surrounding tissues and sometimes the spinal canal. The burst fracture is categorized by the "severity of the deformity, the severity of (spinal) canal compromise, the degree of loss of vertebral body height, and the degree of neurologic deficit." Burst fractures are considered more severe than compression fractures because long-term neurological damage can follow. The neurologic deficits can reach their full extent immediately, or can progress for a prolonged time.

Blunt trauma, also known as blunt force trauma or non-penetrating trauma, is physical trauma or impactful force to a body part, often occurring with road traffic collisions, direct blows, assaults, injuries during sports, and particularly in the elderly who fall. It is contrasted with penetrating trauma which occurs when an object pierces the skin and enters a tissue of the body, creating an open wound and bruise.

Vertebral artery dissection (VAD) is a flap-like tear of the inner lining of the vertebral artery, which is located in the neck and supplies blood to the brain. After the tear, blood enters the arterial wall and forms a blood clot, thickening the artery wall and often impeding blood flow. The symptoms of vertebral artery dissection include head and neck pain and intermittent or permanent stroke symptoms such as difficulty speaking, impaired coordination and visual loss. It is usually diagnosed with a contrast-enhanced CT or MRI scan.

A spinal disc herniation is an injury to the cushioning and connective tissue between vertebrae, usually caused by excessive strain or trauma to the spine. It may result in back pain, pain or sensation in different parts of the body, and physical disability. The most conclusive diagnostic tool for disc herniation is MRI, and treatment may range from painkillers to surgery. Protection from disc herniation is best provided by core strength and an awareness of body mechanics including posture.
Atlanto-occipital dislocation, orthopedic decapitation, or internal decapitation describes ligamentous separation of the spinal column from the skull base. It is possible for a human to survive such an injury; however, 70% of cases result in immediate death. It should not be confused with atlanto-axial dislocation, which describes ligamentous separation between the first and second cervical vertebra.

Projectional radiography, also known as conventional radiography, is a form of radiography and medical imaging that produces two-dimensional images by X-ray radiation. The image acquisition is generally performed by radiographers, and the images are often examined by radiologists. Both the procedure and any resultant images are often simply called 'X-ray'. Plain radiography or roentgenography generally refers to projectional radiography. Plain radiography can also refer to radiography without a radiocontrast agent or radiography that generates single static images, as contrasted to fluoroscopy, which are technically also projectional.

A compression fracture is a collapse of a vertebra. It may be due to trauma or due to a weakening of the vertebra. This weakening is seen in patients with osteoporosis or osteogenesis imperfecta, lytic lesions from metastatic or primary tumors, or infection. In healthy patients, it is most often seen in individuals suffering extreme vertical shocks, such as ejecting from an ejection seat. Seen in lateral views in plain x-ray films, compression fractures of the spine characteristically appear as wedge deformities, with greater loss of height anteriorly than posteriorly and intact pedicles in the anteroposterior view.

The prevertebral space is a space in the neck.

A spinal fracture, also called a vertebral fracture or a broken back, is a fracture affecting the vertebrae of the spinal column. Most types of spinal fracture confer a significant risk of spinal cord injury. After the immediate trauma, there is a risk of spinal cord injury if the fracture is unstable, that is, likely to change alignment without internal or external fixation.
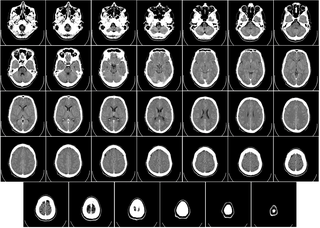
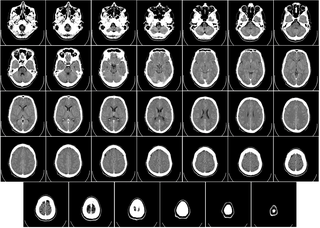
Computed tomography of the head uses a series of X-rays in a CT scan of the head taken from many different directions; the resulting data is transformed into a series of cross sections of the brain using a computer program. CT images of the head are used to investigate and diagnose brain injuries and other neurological conditions, as well as other conditions involving the skull or sinuses; it used to guide some brain surgery procedures as well. CT scans expose the person getting them to ionizing radiation which has a risk of eventually causing cancer; some people have allergic reactions to contrast agents that are used in some CT procedures.

In organized athletics, few situations give rise to greater anxiety than the 'downed athlete'. Obvious causes include head and neck injury, or both, with no immediate means of excluding neck injury in the athlete who may be unable to give a history.
Spinal cord injury without radiographic abnormality (SCIWORA) is symptoms of a spinal cord injury (SCI) with no evidence of injury to the spinal column on X-rays or CT scan. Symptoms may include numbness, weakness, abnormal reflexes, or loss of bladder or bowel control. Neck or back pain is also common. Symptoms may be brief or persistent. Some do not develop symptoms until a few days after the injury.