Related Research Articles
In neuroscience, an F wave is one of several motor responses which may follow the direct motor response (M) evoked by electrical stimulation of peripheral motor or mixed nerves. F-waves are the second of two late voltage changes observed after stimulation is applied to the skin surface above the distal region of a nerve, in addition to the H-reflex which is a muscle reaction in response to electrical stimulation of innervating sensory fibers. Traversal of F-waves along the entire length of peripheral nerves between the spinal cord and muscle, allows for assessment of motor nerve conduction between distal stimulation sites in the arm and leg, and related motoneurons (MN's) in the cervical and lumbosacral cord. F-waves are able to assess both afferent and efferent loops of the alpha motor neuron in its entirety. As such, various properties of F-wave motor nerve conduction are analyzed in nerve conduction studies (NCS), and often used to assess polyneuropathies, resulting from states of neuronal demyelination and loss of peripheral axonal integrity.

The human leg is the entire lower limb of the human body, including the foot, thigh or sometimes even the hip or buttock region. The major bones of the leg are the femur, tibia, and adjacent fibula. The thigh is between the hip and knee, while the calf (rear) and shin (front) are between the knee and foot.
Spasticity is a feature of altered skeletal muscle performance with a combination of paralysis, increased tendon reflex activity, and hypertonia. It is also colloquially referred to as an unusual "tightness", stiffness, or "pull" of muscles.

Tetraplegia, also known as quadriplegia, is defined as the dysfunction or loss of motor and/or sensory function in the cervical area of the spinal cord. A loss of motor function can present as either weakness or paralysis leading to partial or total loss of function in the arms, legs, trunk, and pelvis; paraplegia is similar but affects the thoracic, lumbar, and sacral segments of the spinal cord and arm function is spared. The paralysis may be flaccid or spastic. A loss of sensory function can present as an impairment or complete inability to sense light touch, pressure, heat, pinprick/pain, and proprioception. In these types of spinal cord injury, it is common to have a loss of both sensation and motor control.
The ankle jerk reflex, also known as the Achilles reflex, occurs when the Achilles tendon is tapped while the foot is dorsiflexed. It is a type of stretch reflex that tests the function of the gastrocnemius muscle and the nerve that supplies it. A positive result would be the jerking of the foot towards its plantar surface. Being a deep tendon reflex, it is monosynaptic. It is also a stretch reflex. These are monosynaptic spinal segmental reflexes. When they are intact, integrity of the following is confirmed: cutaneous innervation, motor supply, and cortical input to the corresponding spinal segment.

The patellar reflex, also called the knee reflex or knee-jerk, is a stretch reflex which tests the L2, L3, and L4 segments of the spinal cord. Many animals, most significantly humans, have been seen to have the patellar reflex, including dogs, cats, horses, and other mammalian species.

An upper motor neuron lesion Is an injury or abnormality that occurs in the neural pathway above the anterior horn cell of the spinal cord or motor nuclei of the cranial nerves. Conversely, a lower motor neuron lesion affects nerve fibers traveling from the anterior horn of the spinal cord or the cranial motor nuclei to the relevant muscle(s).

Upper motor neurons (UMNs) is a term introduced by William Gowers in 1886. They are found in the cerebral cortex and brainstem and carry information down to activate interneurons and lower motor neurons, which in turn directly signal muscles to contract or relax. UMNs represent the major origin point for voluntary somatic movement.
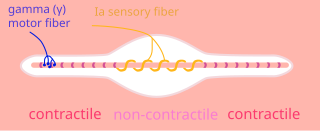
A gamma motor neuron, also called gamma motoneuron, or fusimotor neuron, is a type of lower motor neuron that takes part in the process of muscle contraction, and represents about 30% of (Aγ) fibers going to the muscle. Like alpha motor neurons, their cell bodies are located in the anterior grey column of the spinal cord. They receive input from the reticular formation of the pons in the brainstem. Their axons are smaller than those of the alpha motor neurons, with a diameter of only 5 μm. Unlike the alpha motor neurons, gamma motor neurons do not directly adjust the lengthening or shortening of muscles. However, their role is important in keeping muscle spindles taut, thereby allowing the continued firing of alpha neurons, leading to muscle contraction. These neurons also play a role in adjusting the sensitivity of muscle spindles.

The gastrocnemius muscle is a superficial two-headed muscle that is in the back part of the lower leg of humans. It is located superficial to the soleus in the posterior (back) compartment of the leg. It runs from its two heads just above the knee to the heel, extending across a total of three joints.

The plantaris is one of the superficial muscles of the superficial posterior compartment of the leg, one of the fascial compartments of the leg.
Hypertonia is a term sometimes used synonymously with spasticity and rigidity in the literature surrounding damage to the central nervous system, namely upper motor neuron lesions. Impaired ability of damaged motor neurons to regulate descending pathways gives rise to disordered spinal reflexes, increased excitability of muscle spindles, and decreased synaptic inhibition. These consequences result in abnormally increased muscle tone of symptomatic muscles. Some authors suggest that the current definition for spasticity, the velocity-dependent over-activity of the stretch reflex, is not sufficient as it fails to take into account patients exhibiting increased muscle tone in the absence of stretch reflex over-activity. They instead suggest that "reversible hypertonia" is more appropriate and represents a treatable condition that is responsive to various therapy modalities like drug or physical therapy.

Foot drop is a gait abnormality in which the dropping of the forefoot happens due to weakness, irritation or damage to the deep fibular nerve, including the sciatic nerve, or paralysis of the muscles in the anterior portion of the lower leg. It is usually a symptom of a greater problem, not a disease in itself. Foot drop is characterized by inability or impaired ability to raise the toes or raise the foot from the ankle (dorsiflexion). Foot drop may be temporary or permanent, depending on the extent of muscle weakness or paralysis and it can occur in one or both feet. In walking, the raised leg is slightly bent at the knee to prevent the foot from dragging along the ground.

The vestibulospinal tract is a neural tract in the central nervous system. Specifically, it is a component of the extrapyramidal system and is classified as a component of the medial pathway. Like other descending motor pathways, the vestibulospinal fibers of the tract relay information from nuclei to motor neurons. The vestibular nuclei receive information through the vestibulocochlear nerve about changes in the orientation of the head. The nuclei relay motor commands through the vestibulospinal tract. The function of these motor commands is to alter muscle tone, extend, and change the position of the limbs and head with the goal of supporting posture and maintaining balance of the body and head.

The stretch reflex, or more accurately "muscle stretch reflex", is a muscle contraction in response to stretching a muscle. The function of the reflex is generally thought be maintaining the muscle at a constant length but the response is often coordinated across multiple muscles and even joints. The term deep tendon reflex is often wrongfully used by many health workers and students to refer to this reflex. "Tendons have little to do with the response, other than being responsible for mechanically transmitting the sudden stretch from the reflex hammer to the muscle spindle. In addition, some muscles with stretch reflexes have no tendons ".
The triceps reflex, a deep tendon reflex, is a reflex that elicits involuntary contraction of the triceps brachii muscle. It is sensed and transmitted by the radial nerve. The reflex is tested as part of the neurological examination to assess the sensory and motor pathways within the C7 and C8 spinal nerves.
Clasp-knife response refers to a Golgi tendon reflex with a rapid decrease in resistance when attempting to flex a joint, usually during a neurological examination. It is one of the characteristic responses of an upper motor neuron lesion. It gets its name from the resemblance between the motion of the limb and the sudden closing of a claspknife after sufficient pressure is applied.
The Golgi tendon reflex (also called inverse stretch reflex, autogenic inhibition, tendon reflex) is an inhibitory effect on the muscle resulting from the muscle tension stimulating Golgi tendon organs (GTO) of the muscle, and hence it is self-induced. The reflex arc is a negative feedback mechanism preventing too much tension on the muscle and tendon. When the tension is extreme, the inhibition can be so great it overcomes the excitatory effects on the muscle's alpha motoneurons causing the muscle to suddenly relax. This reflex is also called the inverse myotatic reflex, because it is the inverse of the stretch reflex.
Upper motor neuron syndrome (UMNS) is the motor control changes that can occur in skeletal muscle after an upper motor neuron lesion.

Cutaneous, superficial, or skin reflexes, are activated by skin receptors and play a valuable role in locomotion, providing quick responses to unexpected environmental challenges. They have been shown to be important in responses to obstacles or stumbling, in preparing for visually challenging terrain, and for assistance in making adjustments when instability is introduced. In addition to the role in normal locomotion, cutaneous reflexes are being studied for their potential in enhancing rehabilitation therapy (physiotherapy) for people with gait abnormalities.
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 Hilder, Joseph M.; Zev W. Rymer (September 1999). "A Stimulation Study of Reflex Instability in Spasticity: Origins of Clonus". IEEE Transactions on Rehabilitation Engineering. 7 (3): 327–340. doi:10.1109/86.788469. PMID 10498378.
- 1 2 3 4 5 Douglas, Wallace M.; Bruce H Ross; Christine K. Thomas (Aug 25, 2005). "Motor unit behaviour during clonus". Journal of Applied Physiology. 99 (6): 2166–2172. CiteSeerX 10.1.1.501.9581 . doi:10.1152/japplphysiol.00649.2005. PMID 16099891. S2CID 8598394.
- 1 2 3 Weisenburg, Theodore H (November 1903). "Triceps, Biceps and Finger Clonus". Journal of Nervous and Mental Disease. 30 (11): 681–683. doi:10.1097/00005053-190311000-00003. S2CID 143749312.
- ↑ Mitchell, John K. (May 1902). "Two unusual forms of clonus: toe clonus and lateral ankle clonus". Journal of Nervous and Mental Disease. 29 (5): 260–261. doi:10.1097/00005053-190205000-00002. S2CID 145648718.
- ↑ Anthony, J; Damasceno, A; Ojjii, D (2016-05-18). "Hypertensive disorders of pregnancy: what the physician needs to know". Cardiovascular Journal of Africa. 27 (2): 104–110. doi:10.5830/CVJA-2016-051. PMC 4928160 . PMID 27213858.
- ↑ Bateson, Gregory (1991). A Sacred Unity: Further Steps To An Ecology of Mind (1st ed.). New York: Cornelia & Michael Bessie. p. 85. ISBN 0-06-250100-3.