The adrenal glands are endocrine glands that produce a variety of hormones including adrenaline and the steroids aldosterone and cortisol. They are found above the kidneys. Each gland has an outer cortex which produces steroid hormones and an inner medulla. The adrenal cortex itself is divided into three main zones: the zona glomerulosa, the zona fasciculata and the zona reticularis.

Cushing's syndrome is a collection of signs and symptoms due to prolonged exposure to glucocorticoids such as cortisol. Signs and symptoms may include high blood pressure, abdominal obesity but with thin arms and legs, reddish stretch marks, a round red face due to facial plethora, a fat lump between the shoulders, weak muscles, weak bones, acne, and fragile skin that heals poorly. Women may have more hair and irregular menstruation. Occasionally there may be changes in mood, headaches, and a chronic feeling of tiredness.
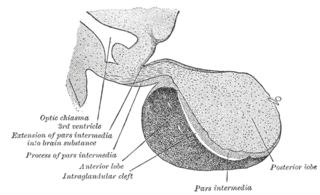
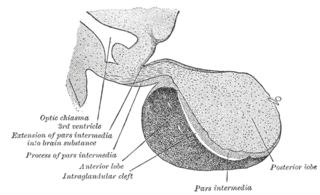
A major organ of the endocrine system, the anterior pituitary is the glandular, anterior lobe that together with the posterior lobe makes up the pituitary gland (hypophysis) which, in humans, is located at the base of the brain, protruding off the bottom of the hypothalamus.

Addison's disease, also known as primary adrenal insufficiency, is a rare long-term endocrine disorder characterized by inadequate production of the steroid hormones cortisol and aldosterone by the two outer layers of the cells of the adrenal glands, causing adrenal insufficiency. Symptoms generally come on slowly and insidiously and may include abdominal pain and gastrointestinal abnormalities, weakness, and weight loss. Darkening of the skin in certain areas may also occur. Under certain circumstances, an adrenal crisis may occur with low blood pressure, vomiting, lower back pain, and loss of consciousness. Mood changes may also occur. Rapid onset of symptoms indicates acute adrenal failure, which is a clinical emergency. An adrenal crisis can be triggered by stress, such as from an injury, surgery, or infection.
Cushing's disease is one cause of Cushing's syndrome characterised by increased secretion of adrenocorticotropic hormone (ACTH) from the anterior pituitary. This is most often as a result of a pituitary adenoma or due to excess production of hypothalamus CRH that stimulates the synthesis of cortisol by the adrenal glands. Pituitary adenomas are responsible for 80% of endogenous Cushing's syndrome, when excluding Cushing's syndrome from exogenously administered corticosteroids. The equine version of this disease is Pituitary pars intermedia dysfunction.

Adrenal insufficiency is a condition in which the adrenal glands do not produce adequate amounts of steroid hormones. The adrenal glands—also referred to as the adrenal cortex—normally secrete glucocorticoids, mineralocorticoids, and androgens. These hormones are important in regulating blood pressure, electrolytes, and metabolism as a whole. Deficiency of these hormones leads to symptoms ranging from abdominal pain, vomiting, muscle weakness and fatigue, low blood pressure, depression, mood and personality changes to organ failure and shock. Adrenal crisis may occur if a person having adrenal insufficiency experiences stresses, such as an accident, injury, surgery, or severe infection; this is a life-threatening medical condition resulting from severe deficiency of cortisol in the body. Death may quickly follow.
Metyrapone, sold under the brand name Metopirone, is a medication which is used in the diagnosis of adrenal insufficiency and occasionally in the treatment of Cushing's syndrome (hypercortisolism). It is part of the steroidogenesis inhibitor class of drugs.

Pituitary adenomas are tumors that occur in the pituitary gland. Most pituitary tumors are benign, approximately 35% are invasive and just 0.1% to 0.2% are carcinomas. Pituitary adenomas represent from 10% to 25% of all intracranial neoplasms and the estimated prevalence rate in the general population is approximately 17%.
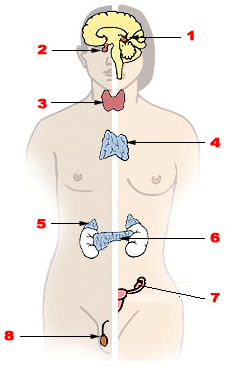
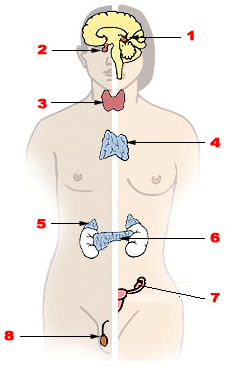
Endocrine glands are ductless glands of the endocrine system that secrete their products, hormones, directly into the blood. The major glands of the endocrine system include the pineal gland, pituitary gland, pancreas, ovaries, testicles, thyroid gland, parathyroid gland, hypothalamus and adrenal glands. The hypothalamus and pituitary glands are neuroendocrine organs.
Nelson's syndrome is a disorder that occurs in about one in four patients who have had both adrenal glands removed to treat Cushing's disease. In patients with pre-existing adrenocorticotropic hormone (ACTH)-secreting pituitary adenomas, loss of adrenal feedback following bilateral adrenalectomy can trigger the rapid growth of the tumor, leading to visual symptoms and hyperpigmentation. The severity of the disease is dependent upon the effect of ACTH release on the skin, pituitary hormone loss from mass compression, as well as invasion into surrounding structures around the pituitary gland.

Mitotane, sold under the brand name Lysodren, is a steroidogenesis inhibitor and cytostatic antineoplastic medication which is used in the treatment of adrenocortical carcinoma and Cushing's syndrome. It is a derivative of the early insecticide DDT and an isomer of p,p'-DDDTooltip dichlorodiphenyldichloroethane (4,4'-dichlorodiphenyldichloroethane) and is also known as 2,4'-(dichlorodiphenyl)-2,2-dichloroethane (o,p'-DDD).
Sudden acquired retinal degeneration syndrome (SARDS) is a disease in dogs causing sudden blindness. It can occur in any breed, but female dogs may be predisposed. Approximately 4000 cases are seen in the United States annually.

The dexamethasone suppression test (DST) is used to assess adrenal gland function by measuring how cortisol levels change in response to oral doses or an injection of dexamethasone. It is typically used to diagnose Cushing's syndrome.
In humans and other animals, the adrenocortical hormones are hormones produced by the adrenal cortex, the outer region of the adrenal gland. These polycyclic steroid hormones have a variety of roles that are crucial for the body's response to stress, and they also regulate other functions in the body. Threats to homeostasis, such as injury, chemical imbalances, infection, or psychological stress, can initiate a stress response. Examples of adrenocortical hormones that are involved in the stress response are aldosterone and cortisol. These hormones also function in regulating the conservation of water by the kidneys and glucose metabolism, respectively.

Trilostane, sold under the brand name Vetoryl among others, is a medication which has been used in the treatment of Cushing's syndrome, Conn's syndrome, and postmenopausal breast cancer in humans. It was withdrawn for use in humans in the United States in the 1990s but was subsequently approved for use in veterinary medicine in the 2000s to treat Cushing's syndrome in dogs. It is taken by mouth.
Corticorelin is a diagnostic agent. It is a synthetic form of human corticotropin-releasing hormone (hCRH).
Hypoadrenocorticism in dogs, or, as it is known in people, Addison's disease, is an endocrine system disorder that occurs when the adrenal glands fail to produce enough hormones for normal function. The adrenal glands secrete glucocorticoids such as cortisol and mineralocorticoids such as aldosterone; when proper amounts of these are not produced, the metabolic and electrolyte balance is upset. Mineralocorticoids control the amount of potassium, sodium, and water in the body. Hypoadrenocorticism is fatal if left untreated.

Adrenal gland disorders are conditions that interfere with the normal functioning of the adrenal glands. Your body produces too much or too little of one or more hormones when you have an adrenal gland dysfunction. The type of issue you have and the degree to which it affects your body's hormone levels determine the symptoms.

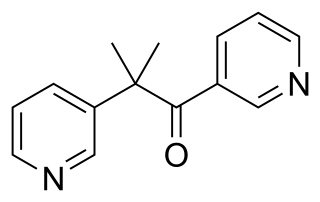
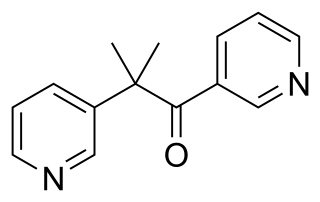
Amphenone B, or simply amphenone, also known as 3,3-bis(p-aminophenyl)butan-2-one, is an inhibitor of steroid hormone and thyroid hormone biosynthesis which was never marketed but has been used as a tool in scientific research to study corticosteroids and the adrenal glands. It acts as competitive inhibitor of 11β-hydroxylase, 17α-hydroxylase, 17,20-lyase, 21-hydroxylase, and 3β-hydroxysteroid dehydrogenase, as well as of cholesterol side-chain cleavage enzyme, thereby inhibiting the production of steroid hormones including glucocorticoids, mineralocorticoids, androgens, and estrogens. In addition, amphenone B inhibits the production of thyroxine by a thiouracil-like mechanism, specifically via inhibition of organic binding of iodine and uptake of iodide by the thyroid gland.

Adrenalism describes the condition of an excessive or substandard secretion of hormones related to the adrenal glands, which are found directly superior to the kidneys. Adrenalism can be further distinguished as hyperadrenalism, referring to the excessive secretion of hormones, and hypoadrenalism, referring to the insufficient secretion of hormones.