Related Research Articles

Otorhinolaryngology is a surgical subspecialty within medicine that deals with the surgical and medical management of conditions of the head and neck. Doctors who specialize in this area are called otorhinolaryngologists, otolaryngologists, head and neck surgeons, or ENT surgeons or physicians. Patients seek treatment from an otorhinolaryngologist for diseases of the ear, nose, throat, base of the skull, head, and neck. These commonly include functional diseases that affect the senses and activities of eating, drinking, speaking, breathing, swallowing, and hearing. In addition, ENT surgery encompasses the surgical management of cancers and benign tumors and reconstruction of the head and neck as well as plastic surgery of the face, scalp, and neck.
Sinusitis, also known as rhinosinusitis, is an inflammation of the mucous membranes that line the sinuses resulting in symptoms that may include thick nasal mucus, a plugged nose, and facial pain.

Nasal polyps (NP) are noncancerous growths within the nose or sinuses. Symptoms include trouble breathing through the nose, loss of smell, decreased taste, post nasal drip, and a runny nose. The growths are sac-like, movable, and nontender, though face pain may occasionally occur. They typically occur in both nostrils in those who are affected. Complications may include sinusitis and broadening of the nose.

Aspirin-exacerbated respiratory disease (AERD), also called NSAID-exacerbated respiratory disease (N-ERD) or historically aspirin-induced asthma and Samter's Triad, is a long-term disease defined by three simultaneous symptoms: asthma, chronic rhinosinusitis with nasal polyps, and intolerance of aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs). Compared to aspirin tolerant patients, AERD patients' asthma and nasal polyps are generally more severe. Reduction or loss of the ability to smell is extremely common, occurring in more than 90% of people with the disease. AERD most commonly begins in early- to mid-adulthood and has no known cure. While NSAID intolerance is a defining feature of AERD, avoidance of NSAIDs does not affect the onset, development or perennial nature of the disease.

Nasal irrigation is a personal hygiene practice in which the nasal cavity is washed to flush out mucus and debris from the nose and sinuses, in order to enhance nasal breathing. Nasal irrigation can also refer to the use of saline nasal spray or nebulizers to moisten the mucous membranes.

Empty nose syndrome (ENS) is a clinical syndrome, the hallmark symptom of which is a sensation of suffocation despite a clear airway. This syndrome is often referred to as a form of secondary atrophic rhinitis. ENS is a potential complication of nasal turbinate surgery or injury. Patients have usually undergone a turbinectomy or other surgical procedures that injure the nasal turbinates.
Balloon sinuplasty is a procedure that ear, nose and throat surgeons may use for the treatment of blocked sinuses. Patients diagnosed with sinusitis but not responding to medications may be candidates for sinus surgery. Balloon technology was initially cleared by the U.S. Food and Drug Administration in 2005 and is an endoscopic, catheter-based system for chronic sinusitis. It uses a balloon over a wire catheter to dilate sinus passageways. The balloon is inflated with the goal of dilating the sinus openings, widening the walls of the sinus passageway and restoring normal drainage.

Functional endoscopic sinus surgery (FESS) is a procedure that is used to treat sinusitis and other conditions that affect the sinuses. Sinusitis is an inflammation of the sinuses that can cause symptoms such as congestion, headaches, and difficulty breathing through the nose.

An inverted papilloma, also known as Ringertz tumour, is a type of tumor in which surface epithelial cells grow downward into the underlying supportive tissue. It may occur in the nose and/or sinuses or in the urinary tract. When it occurs in the nose or sinuses, it may cause symptoms similar to those caused by sinusitis, such as nasal congestion. When it occurs in the urinary tract, it may cause blood in the urine.
Endoscopic ear surgery (EES) is a minimally invasive alternative to traditional ear surgery and is defined as the use of the rigid endoscope, as opposed to a surgical microscope, to visualize the middle and inner ear during otologic surgery. During endoscopic ear surgery the surgeon holds the endoscope in one hand while working in the ear with the other. To allow this kind of single-handed surgery, different surgical instruments have to be used. Endoscopic visualization has improved due to high-definition video imaging and wide-field endoscopy, and being less invasive, EES is gaining importance as an adjunct to microscopic ear surgery.
Laryngeal cysts are cysts involving the larynx or more frequently supraglottic locations, such as epiglottis and vallecula. Usually they do not extend to the thyroid cartilage. They may be present congenitally or may develop eventually due to degenerative cause. They often interfere with phonation.
Antral lavage is a largely obsolete surgical procedure in which a cannula is inserted into the maxillary sinus via the inferior meatus to allow irrigation and drainage of the sinus. It is also called proof puncture, as the presence of an infection can be proven during the procedure. Upon presence of infection, it can be considered as therapeutic puncture. Often, multiple repeated lavages are subsequently required to allow for full washout of infection.
Caldwell-Luc surgery, Caldwell-Luc operation, also known as Caldwell-Luc antrostomy, and Radical antrostomy, is an operation to remove irreversibly damaged mucosa of the maxillary sinus. It is done when maxillary sinusitis is not cured by medication or other non-invasive technique. The approach is mainly from the anterior wall of the maxilla bone. It was introduced by George Caldwell (1893)and Henry Luc (1897). The maxillary sinus is entered from two separate openings, one in the canine fossa to gain access to the antrum and other in the naso antral wall for drainage.
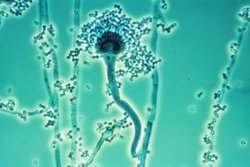
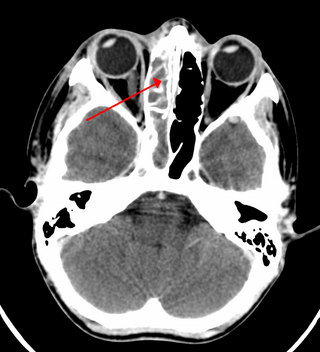
Fungal sinusitis or fungal rhinosinusitis is the inflammation of the lining mucosa of the paranasal sinuses due to a fungal infection. It occurs in people with reduced immunity. The maxillary sinus is the most commonly involved. Fungi responsible for fungal sinusitis are Aspergillus fumigatus (90%), Aspergillus flavus, and Aspergillus niger. Fungal sinusitis occurs most commonly in middle-aged populations. Diabetes mellitus is the most common risk factor involved.
Claire Hopkins is a British Ear, Nose & Throat (ENT) surgeon at Guy's Hospital and Professor of Rhinology at King's College London. She is the President of the British Rhinological Society. During the COVID-19 pandemic, Hopkins successfully campaigned to have anosmia recognised as a symptom of COVID-19 in the United Kingdom.
C. William Hanson, III is an American internist, anesthesiologist and intensivist as well as an academic, author and researcher. He is a Professor of Anesthesiology and Critical Care, Surgery and Internal Medicine at the Hospital of University of Pennsylvania and Professor of Computer and Information Science in the School of Engineering and Applied Science at the University of Pennsylvania. He is also the Chief Medical Information Officer of the University of Pennsylvania Health System.
Nasal surgery is a medical procedure designed to treat various conditions that cause nasal blockages in the upper respiratory tract, for example nasal polyps, inferior turbinate hypertrophy, and chronic rhinosinusitis. It encompasses several types of techniques, including rhinoplasty, septoplasty, sinus surgery, and turbinoplasty, each with its respective postoperative treatments. Furthermore, nasal surgery is also conducted for cosmetic purposes. While there are potential risks and complications associated, the advancement of medical instruments and enhanced surgical skills have helped mitigate them.

Odontogenic sinusitis is a type of sinusitis, specifically caused by dental infections or procedures. Comprising approximately 10-12% of all chronic sinusitis cases, this condition primarily affects the maxillary sinus, which is in close proximity to the upper teeth.
Mary Despina Lekas Picozzi was an American physician. She was head of otolaryngology and Surgeon-in-Chief at Rhode Island Hospital from 1983 to 1996, professor of Clinical Otolaryngology at Brown University's Alpert Medical School, and president of the New England Otolaryngological Society.

Dame Valerie Joan Lund is a British surgeon and emeritus Professor in Rhinology at University College London. Lund has worked on endoscopic endonasal surgery and studies sinonasal conditions She was elevated from CBE to DBE in the 2024 New Year Honours.
References
- ↑ "New medical app for doctors, patients' families | ABC7 Chicago | abc7chicago.com". ABC7 Chicago.
- ↑ Abelson, Reed (May 4, 2006). "Too Soon to Breathe Easy?". The New York Times– via NYTimes.com.
- ↑ https://www.washingtonpost.com/archive/lifestyle/wellness/1993/11/30/sinuses/160ba22e-d3f0-49bf-86f7-39ac84d4f78f/
- ↑ "Book Excerpt: A Saga Of 'Fishy' Surgery For Chronic Sinus Trouble". www.wbur.org. March 2, 2012.
- ↑ https://www.med.upenn.edu/endowedprofessorships/the-david-w-kennedy-md-professorship.html
- 1 2 3 4 "David W. Kennedy - Faculty Biosketch". www.med.upenn.edu.
- 1 2 "Alumni Awards 2022". issuu.
- 1 2 3 4 https://www.hopkinsmedicine.org/otolaryngology/specialty-areas/sinus-center/history
- ↑ Kane, K. J. (January 2020). "The early history and development of functional endoscopic sinus surgery". The Journal of Laryngology and Otology. 134 (1): 8–13. doi:10.1017/S0022215119002457. ISSN 1748-5460. PMID 31831081.
- 1 2 3 https://www.med.upenn.edu/apps/faculty/index.php/g329/p18996
- 1 2 http://www.ampleforthjournal.org/V_103.pdf
- 1 2 3 "The David W. Kennedy, MD Professorship | Endowed Professorships | Perelman School of Medicine at the University of Pennsylvania". www.med.upenn.edu.
- ↑ https://www.washingtonpost.com/archive/lifestyle/wellness/1990/02/06/sudden-pain-in-the-jaw-it-may-not-be-your-teeth/30e6f2ee-97d1-4ed8-a80a-8f4918a8866b/
- 1 2 3 https://www.uab.edu/medicine/otolaryngology/images/documents/hicks-2015.pdf
- ↑ "The David W. Kennedy, MD Professorship | Endowed Professorships | Perelman School of Medicine at the University of Pennsylvania".
- ↑ Smith, T. L. (2017). "THE 2017 13(TH) ANNUAL DAVID W. KENNEDY, MD, LECTURE the evolution of outcomes in sinus surgery for chronic rhinosinusitis: Past, present, and future". International Forum of Allergy & Rhinology. 7 (12): 1121–1126. doi:10.1002/alr.22026. PMC 5716851 . PMID 29028274.
- ↑ https://jamanetwork.com/journals/jamaotolaryngology/article-abstract/615255