Diagnosis
| | This section is empty. You can help by adding to it. (October 2017) |
| Diabetic angiopathy | |
|---|---|
| Specialty | Diabetology, angiology |
Diabetic angiopathy is a form of angiopathy associated with diabetic complications. [1] While not exclusive, the two most common forms are diabetic retinopathy and diabetic nephropathy, whose pathophysiologies are largely identical. Other forms of diabetic angiopathy include diabetic neuropathy and diabetic cardiomyopathy. [2] [3]
Diabetes mellitus is the most common cause of adult kidney failure worldwide. It also the most common cause of amputation in the US, usually toes and feet, often as a result of gangrene, and almost always as a result of peripheral artery disease. Retinal damage (from microangiopathy) makes it the most common cause of blindness among non-elderly adults in the US.[ citation needed ]
As insulin is required for glucose uptake, hyperglycemia in diabetes mellitus does not result in a net increase in intracellular glucose in most cells. However, chronic dysregulated blood glucose in diabetes is toxic to cells of the vascular endothelium which passively assimilate glucose. That is, cells in which insulin is not required for intercellular transport of glucose, most-notably the pericytes of the microvasculature. In addition to direct glucose-induced damage by (e.g.) glycation, [4] pericytes, express enzymes which convert glucose into osmotically active metabolites such as sorbitol leading to hypertonic cell lysis. [5] The enzyme, namely aldose reductase, is also expressed in the endothelial and Schwann cells of the peripheral nervous system, contributing to diabetic neuropathy. [6]
Over time, pericyte death may result in reduced capillary integrity; subsequently, there is leaking of albumin and other proteins into fluid compartments. The glomeruli of the kidneys are especially sensitive – see diabetic nephropathy – where protein leakage caused by late-stage angiopathy results in diagnostic proteinuria and eventually kidney failure. In diabetic retinopathy the end-result is often blindness due to irreversible retinal damage. [7]
| | This section is empty. You can help by adding to it. (October 2017) |
| | This section is empty. You can help by adding to it. (October 2017) |
Prognosis is generally poor for all forms of diabetic angiopathy, as symptomatology is tied to the advancement of the underlying pathology i.e. the early-stage patient displays either non-specific symptoms or none at all.[ citation needed ]
"Diabetic dermopathy" is a manifestation of diabetic angiopathy. It is often found on the shin.There is also neuropathy; also associated with diabetes mellitus; type 1 and 2.[ citation needed ]
The following is a glossary of diabetes which explains terms connected with diabetes.
Angiopathy is the generic term for a disease of the blood vessels. The best known and most prevalent angiopathy is diabetic angiopathy, a common complication of chronic diabetes.
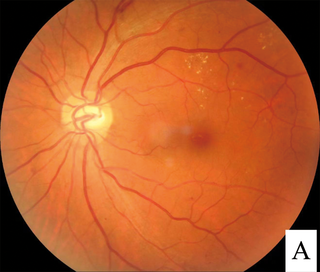
Diabetic retinopathy, is a medical condition in which damage occurs to the retina due to diabetes mellitus. It is a leading cause of blindness in developed countries.

Microangiopathy is a disease of the microvessels, small blood vessels in the microcirculation. It can be contrasted to macroangiopathies such as atherosclerosis, where large and medium-sized arteries are primarily affected.

The connecting peptide, or C-peptide, is a short 31-amino-acid polypeptide that connects insulin's A-chain to its B-chain in the proinsulin molecule. In the context of diabetes or hypoglycemia, a measurement of C-peptide blood serum levels can be used to distinguish between different conditions with similar clinical features.
Diabetic neuropathy is various types of nerve damage associated with diabetes mellitus. Symptoms depend on the site of nerve damage and can include motor changes such as weakness; sensory symptoms such as numbness, tingling, or pain; or autonomic changes such as urinary symptoms. These changes are thought to result from a microvascular injury involving small blood vessels that supply nerves. Relatively common conditions which may be associated with diabetic neuropathy include distal symmetric polyneuropathy; third, fourth, or sixth cranial nerve palsy; mononeuropathy; mononeuropathy multiplex; diabetic amyotrophy; and autonomic neuropathy.

Peripheral neuropathy, often shortened to neuropathy, is a general term describing damage or disease affecting the nerves. Damage to nerves may impair sensation, movement, gland function, and/or organ function depending on which nerves are affected. Neuropathy affecting motor, sensory, or autonomic nerves result in different symptoms. More than one type of nerve may be affected simultaneously. Peripheral neuropathy may be acute or chronic, and may be reversible or permanent.
Glycated hemoglobin is a form of hemoglobin (Hb) that is chemically linked to a sugar. Most monosaccharides, including glucose, galactose and fructose, spontaneously bond with hemoglobin when present in the bloodstream. However, glucose is less likely to do so than galactose and fructose, which may explain why glucose is used as the primary metabolic fuel in humans.
A complication in medicine, or medical complication, is an unfavorable result of a disease, health condition, or treatment. Complications may adversely affect the prognosis, or outcome, of a disease. Complications generally involve a worsening in the severity of the disease or the development of new signs, symptoms, or pathological changes that may become widespread throughout the body and affect other organ systems. Thus, complications may lead to the development of new diseases resulting from previously existing diseases. Complications may also arise as a result of various treatments.

Diabetic nephropathy, also known as diabetic kidney disease, is the chronic loss of kidney function occurring in those with diabetes mellitus. Diabetic nephropathy is the leading causes of chronic kidney disease (CKD) and end-stage renal disease (ESRD) globally. The triad of protein leaking into the urine, rising blood pressure with hypertension and then falling renal function is common to many forms of CKD. Protein loss in the urine due to damage of the glomeruli may become massive, and cause a low serum albumin with resulting generalized body swelling (edema) so called nephrotic syndrome. Likewise, the estimated glomerular filtration rate (eGFR) may progressively fall from a normal of over 90 ml/min/1.73m2 to less than 15, at which point the patient is said to have end-stage renal disease. It usually is slowly progressive over years.

Type 1 diabetes (T1D), formerly known as juvenile diabetes, is an autoimmune disease that originates when cells that make insulin are destroyed by the immune system. Insulin is a hormone required for the cells to use blood sugar for energy and it helps regulate glucose levels in the bloodstream. Before treatment this results in high blood sugar levels in the body. The common symptoms of this elevated blood sugar are frequent urination, increased thirst, increased hunger, weight loss, and other serious complications. Additional symptoms may include blurry vision, tiredness, and slow wound healing. Symptoms typically develop over a short period of time, often a matter of weeks if not months.
The term diabetes includes several different metabolic disorders that all, if left untreated, result in abnormally high concentrations of a sugar called glucose in the blood. Diabetes mellitus type 1 results when the pancreas no longer produces significant amounts of the hormone insulin, usually owing to the autoimmune destruction of the insulin-producing beta cells of the pancreas. Diabetes mellitus type 2, in contrast, is now thought to result from autoimmune attacks on the pancreas and/or insulin resistance. The pancreas of a person with type 2 diabetes may be producing normal or even abnormally large amounts of insulin. Other forms of diabetes mellitus, such as the various forms of maturity-onset diabetes of the young, may represent some combination of insufficient insulin production and insulin resistance. Some degree of insulin resistance may also be present in a person with type 1 diabetes.

For pregnant women with diabetes, some particular challenges exist for both mother and fetus. If the pregnant woman has diabetes as a pre-existing disorder, it can cause early labor, birth defects, and larger than average infants. Therefore, experts advise diabetics to maintain blood sugar level close to normal range about 3 months before planning for pregnancy.
Proximal diabetic neuropathy, also known as diabetic amyotrophy, is a complication of diabetes mellitus that affects the nerves that supply the thighs, hips, buttocks and/or lower legs. Proximal diabetic neuropathy is a type of diabetic neuropathy characterized by muscle wasting, weakness, pain, or changes in sensation/numbness of the leg. It is caused by damage to the nerves of the lumbosacral plexus.
The polyol pathway is a two-step process that converts glucose to fructose. In this pathway glucose is reduced to sorbitol, which is subsequently oxidized to fructose. It is also called the sorbitol-aldose reductase pathway.

Benfotiamine is a synthetic, fat-soluble, S-acyl derivative of thiamine that is approved in some countries as a medication or dietary supplement to treat diabetic sensorimotor polyneuropathy. Benfotiamine was developed in late 1950s in Japan.
Complications of diabetes are secondary diseases that are a result of elevated blood glucose levels that occur in diabetic patients. These complications can be divided into two types: acute and chronic. Acute complications are complications that develop rapidly and can be exemplified as diabetic ketoacidosis (DKA), hyperglycemic hyperosmolar state (HHS), lactic acidosis (LA), and hypoglycemia. Chronic complications develop over time and are generally classified in two categories: microvascular and macrovascular. Microvascular complications include neuropathy, nephropathy, and retinopathy; while cardiovascular disease, stroke, and peripheral vascular disease are included in the macrovascular complications.
In recent years it has become apparent that the environment and underlying mechanisms affect gene expression and the genome outside of the central dogma of biology. It has been found that many epigenetic mechanisms are involved in the regulation and expression of genes such as DNA methylation and chromatin remodeling. These epigenetic mechanisms are believed to be a contributing factor to pathological diseases such as type 2 diabetes. An understanding of the epigenome of Diabetes patients may help to elucidate otherwise hidden causes of this disease.

Diabetes mellitus, often known simply as diabetes, is a group of common endocrine diseases characterized by sustained high blood sugar levels. Diabetes is due to either the pancreas not producing enough insulin, or the cells of the body becoming unresponsive to the hormone's effects. Classic symptoms include thirst, polyuria, weight loss, and blurred vision. If left untreated, the disease can lead to various health complications, including disorders of the cardiovascular system, eye, kidney, and nerves. Untreated or poorly treated diabetes accounts for approximately 1.5 million deaths every year.
Type 3c diabetes is diabetes that comes secondary to pancreatic diseases, involving the exocrine and digestive functions of the pancreas. It also occurs following surgical removal of the pancreas.