Acetazolamide, sold under the trade name Diamox among others, is a medication used to treat glaucoma, epilepsy, altitude sickness, periodic paralysis, idiopathic intracranial hypertension, urine alkalinization, and heart failure. It may be used long term for the treatment of open angle glaucoma and short term for acute angle closure glaucoma until surgery can be carried out. It is taken by mouth or injection into a vein. Acetazolamide is a first generation carbonic anhydrase inhibitor and it decreases the ocular fluid and osmolality in the eye to decrease intraocular pressure.

The collecting duct system of the kidney consists of a series of tubules and ducts that physically connect nephrons to a minor calyx or directly to the renal pelvis. The collecting duct system is the last part of nephron and participates in electrolyte and fluid balance through reabsorption and excretion, processes regulated by the hormones aldosterone and vasopressin.

Renal physiology is the study of the physiology of the kidney. This encompasses all functions of the kidney, including maintenance of acid-base balance; regulation of fluid balance; regulation of sodium, potassium, and other electrolytes; clearance of toxins; absorption of glucose, amino acids, and other small molecules; regulation of blood pressure; production of various hormones, such as erythropoietin; and activation of vitamin D.

Metabolic acidosis is a serious electrolyte disorder characterized by an imbalance in the body's acid-base balance. Metabolic acidosis has three main root causes: increased acid production, loss of bicarbonate, and a reduced ability of the kidneys to excrete excess acids. Metabolic acidosis can lead to acidemia, which is defined as arterial blood pH that is lower than 7.35. Acidemia and acidosis are not mutually exclusive – pH and hydrogen ion concentrations also depend on the coexistence of other acid-base disorders; therefore, pH levels in people with metabolic acidosis can range from low to high.

Potassium-sparing diuretics refers to drugs that cause diuresis without causing potassium loss in the urine. They are typically used as an adjunct in management of hypertension, cirrhosis, and congestive heart failure. The steroidal aldosterone antagonists can also be used for treatment of primary hyperaldosteronism. Spironolactone, a steroidal aldosterone antagonist, is also used in management of female hirsutism and acne from PCOS or other causes.
The anion gap is a value calculated from the results of multiple individual medical lab tests. It may be reported with the results of an electrolyte panel, which is often performed as part of a comprehensive metabolic panel.

Metabolic alkalosis is a metabolic condition in which the pH of tissue is elevated beyond the normal range (7.35–7.45). This is the result of decreased hydrogen ion concentration, leading to increased bicarbonate, or alternatively a direct result of increased bicarbonate concentrations. The condition typically cannot last long if the kidneys are functioning properly.

Hyperaldosteronism is a medical condition wherein too much aldosterone is produced by the adrenal glands, which can lead to lowered levels of potassium in the blood (hypokalemia) and increased hydrogen ion excretion (alkalosis).

Renal tubular acidosis (RTA) is a medical condition that involves an accumulation of acid in the body due to a failure of the kidneys to appropriately acidify the urine. In renal physiology, when blood is filtered by the kidney, the filtrate passes through the tubules of the nephron, allowing for exchange of salts, acid equivalents, and other solutes before it drains into the bladder as urine. The metabolic acidosis that results from RTA may be caused either by insufficient secretion of hydrogen ions into the latter portions of the nephron or by failure to reabsorb sufficient bicarbonate ions from the filtrate in the early portion of the nephron. Although a metabolic acidosis also occurs in those with chronic kidney disease, the term RTA is reserved for individuals with poor urinary acidification in otherwise well-functioning kidneys. Several different types of RTA exist, which all have different syndromes and different causes. RTA is usually an incidental finding based on routine blood draws that show abnormal results. Clinically, patients may present with vague symptoms such as dehydration, mental status changes, or delayed growth in adolescents.

Bartter syndrome (BS) is a rare inherited disease characterised by a defect in the thick ascending limb of the loop of Henle, which results in low potassium levels (hypokalemia), increased blood pH (alkalosis), and normal to low blood pressure. There are two types of Bartter syndrome: neonatal and classic. A closely associated disorder, Gitelman syndrome, is milder than both subtypes of Bartter syndrome.

Oculocerebrorenal syndrome is a rare X-linked recessive disorder characterized by congenital cataracts, hypotonia, intellectual disability, proximal tubular acidosis, aminoaciduria and low-molecular-weight proteinuria. Lowe syndrome can be considered a cause of Fanconi syndrome.

Dent's disease is a rare X-linked recessive inherited condition that affects the proximal renal tubules of the kidney. It is one cause of Fanconi syndrome, and is characterized by tubular proteinuria, excess calcium in the urine, formation of calcium kidney stones, nephrocalcinosis, and chronic kidney failure.
Nephrocalcinosis, once known as Albright's calcinosis after Fuller Albright, is a term originally used to describe deposition of calcium salts in the renal parenchyma due to hyperparathyroidism. The term nephrocalcinosis is used to describe the deposition of both calcium oxalate and calcium phosphate. It may cause acute kidney injury. It is now more commonly used to describe diffuse, fine, renal parenchymal calcification in radiology. It is caused by multiple different conditions and is determined progressive kidney dysfunction. These outlines eventually come together to form a dense mass. During its early stages, nephrocalcinosis is visible on x-ray, and appears as a fine granular mottling over the renal outlines. It is most commonly seen as an incidental finding with medullary sponge kidney on an abdominal x-ray. It may be severe enough to cause renal tubular acidosis or even end stage kidney disease, due to disruption of the kidney tissue by the deposited calcium.

Medullary sponge kidney is a congenital disorder of the kidneys characterized by cystic dilatation of the collecting tubules in one or both kidneys. Individuals with medullary sponge kidney are at increased risk for kidney stones and urinary tract infection (UTI). Patients with MSK typically pass twice as many stones per year as do other stone formers without MSK. While having a low morbidity rate, as many as 10% of patients with MSK have an increased risk of morbidity associated with frequent stones and UTIs. While many patients report increased chronic kidney pain, the source of the pain, when a UTI or blockage is not present, is unclear at this time. Renal colic is present in 55% of patients. Women with MSK experience more stones, UTIs, and complications than men. MSK was previously believed not to be hereditary but there is more evidence coming forth that may indicate otherwise.
Lightwood–Albright syndrome is a neonatal form of renal tubular acidosis. It is characterized by distal renal tubular acidosis that occurs as a result of bicarbonate wasting and the inability to excrete hydrogen ions. By definition, it is a transient process and has no particular disease course. If untreated, it may lead to nephrocalcinosis and failure to thrive.
The urine anion gap is calculated using measured ions found in the urine. It is used to aid in the differential diagnosis of metabolic acidosis.
Fanconi syndrome or Fanconi's syndrome is a syndrome of inadequate reabsorption in the proximal renal tubules of the kidney. The syndrome can be caused by various underlying congenital or acquired diseases, by toxicity, or by adverse drug reactions. It results in various small molecules of metabolism being passed into the urine instead of being reabsorbed from the tubular fluid. Fanconi syndrome affects the proximal tubules, namely, the proximal convoluted tubule (PCT), which is the first part of the tubule to process fluid after it is filtered through the glomerulus, and the proximal straight tubule, which leads to the descending limb of loop of Henle.
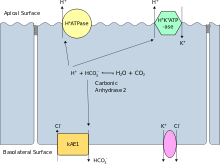
Proximal renal tubular acidosis (pRTA) or type 2 renal tubular acidosis (RTA) is a type of RTA caused by a failure of the proximal tubular cells to reabsorb filtered bicarbonate from the urine, leading to urinary bicarbonate wasting and subsequent acidemia. The distal intercalated cells function normally, so the acidemia is less severe than dRTA and the urine can acidify to a pH of less than 5.3. pRTA also has several causes, and may occasionally be present as a solitary defect, but is usually associated with a more generalised dysfunction of the proximal tubular cells called Fanconi syndrome where there is also phosphaturia, glycosuria, aminoaciduria, uricosuria and tubular proteinuria.

Professor Oliver Murray Wrong was an eminent academic nephrologist and one of the founders of the speciality in the United Kingdom. From a background as a "salt and water" physician, he made detailed clinical observations and scientifically imaginative connections which were the basis of numerous advances in the molecular biology of the human kidney. Wrong himself contributed to much of the molecular work after his own "retirement". He dictated amendments to his final paper during his final illness in his own teaching hospital, University College Hospital (UCH), London. Though academic in his leanings, he was a compassionate physician who established a warm rapport with patients, a link he regarded as the keystone of his research. He belonged to a generation of idealistic young doctors responsible for the establishment of the UK's National Health Service in the post-War years.

Renal stone formation and passage during space flight can potentially pose a severe risk to crew member health and safety and could affect mission outcome. Although renal stones are routinely and successfully treated on Earth, the occurrence of these during space flight can prove to be problematic.