Autosomal dominant polycystic kidney disease (ADPKD) is one of the most common, life-threatening inherited human disorders and the most common hereditary kidney disease. It is associated with large interfamilial and intrafamilial variability, which can be explained to a large extent by its genetic heterogeneity and modifier genes. It is also the most common of the inherited cystic kidney diseases — a group of disorders with related but distinct pathogenesis, characterized by the development of renal cysts and various extrarenal manifestations, which in case of ADPKD include cysts in other organs, such as the liver, seminal vesicles, pancreas, and arachnoid membrane, as well as other abnormalities, such as intracranial aneurysms and dolichoectasias, aortic root dilatation and aneurysms, mitral valve prolapse, and abdominal wall hernias. Over 50% of patients with ADPKD eventually develop end stage kidney disease and require dialysis or kidney transplantation. ADPKD is estimated to affect at least one in every 1000 individuals worldwide, making this disease the most common inherited kidney disorder with a diagnosed prevalence of 1:2000 and incidence of 1:3000-1:8000 in a global scale.

Proteinuria is the presence of excess proteins in the urine. In healthy persons, urine contains very little protein, less than 150 mg/day; an excess is suggestive of illness. Excess protein in the urine often causes the urine to become foamy. Severe proteinuria can cause nephrotic syndrome in which there is worsening swelling of the body.

Kidney failure, also known as end-stage kidney disease, is a medical condition in which the kidneys can no longer adequately filter waste products from the blood, functioning at less than 15% of normal levels. Kidney failure is classified as either acute kidney failure, which develops rapidly and may resolve; and chronic kidney failure, which develops slowly and can often be irreversible. Symptoms may include leg swelling, feeling tired, vomiting, loss of appetite, and confusion. Complications of acute and chronic failure include uremia, hyperkalaemia, and volume overload. Complications of chronic failure also include heart disease, high blood pressure, and anaemia.

Chronic kidney disease (CKD) is a type of kidney disease in which a gradual loss of kidney function occurs over a period of months to years. Initially generally no symptoms are seen, but later symptoms may include leg swelling, feeling tired, vomiting, loss of appetite, and confusion. Complications can relate to hormonal dysfunction of the kidneys and include high blood pressure, bone disease, and anemia. Additionally CKD patients have markedly increased cardiovascular complications with increased risks of death and hospitalization.

IgA nephropathy (IgAN), also known as Berger's disease, or synpharyngitic glomerulonephritis, is a disease of the kidney and the immune system; specifically it is a form of glomerulonephritis or an inflammation of the glomeruli of the kidney. Aggressive Berger's disease can attack other major organs, such as the liver, skin and heart.

Metabolic acidosis is a serious electrolyte disorder characterized by an imbalance in the body's acid-base balance. Metabolic acidosis has three main root causes: increased acid production, loss of bicarbonate, and a reduced ability of the kidneys to excrete excess acids. Metabolic acidosis can lead to acidemia, which is defined as arterial blood pH that is lower than 7.35. Acidemia and acidosis are not mutually exclusive – pH and hydrogen ion concentrations also depend on the coexistence of other acid-base disorders; therefore, pH levels in people with metabolic acidosis can range from low to high.

Diabetic nephropathy, also known as diabetic kidney disease, is the chronic loss of kidney function occurring in those with diabetes mellitus. Diabetic nephropathy is the leading causes of chronic kidney disease (CKD) and end-stage renal disease (ESRD) globally. The triad of protein leaking into the urine, rising blood pressure with hypertension and then falling renal function is common to many forms of CKD. Protein loss in the urine due to damage of the glomeruli may become massive, and cause a low serum albumin with resulting generalized body swelling (edema) so called nephrotic syndrome. Likewise, the estimated glomerular filtration rate (eGFR) may progressively fall from a normal of over 90 ml/min/1.73m2 to less than 15, at which point the patient is said to have end-stage renal disease. It usually is slowly progressive over years.

Membranous glomerulonephritis (MGN) is a slowly progressive disease of the kidney affecting mostly people between ages of 30 and 50 years, usually white people.
Protein toxicity is the effect of the buildup of protein metabolic waste compounds, like urea, uric acid, ammonia, and creatinine. Protein toxicity has many causes, including urea cycle disorders, genetic mutations, excessive protein intake, and insufficient kidney function, such as chronic kidney disease and acute kidney injury. Symptoms of protein toxicity include unexplained vomiting and loss of appetite. Untreated protein toxicity can lead to serious complications such as seizures, encephalopathy, further kidney damage, and even death.
Interstitial nephritis, also known as tubulointerstitial nephritis, is inflammation of the area of the kidney known as the renal interstitium, which consists of a collection of cells, extracellular matrix, and fluid surrounding the renal tubules. It is also known as intestinal nephritis because the clinical picture may include mesenteric lymphadenitis in some cases of acute pyelonephritis. More specifically, in case of recurrent urinary tract infection, secondary infection can spread to adjacent intestine. In addition to providing a scaffolding support for the tubular architecture, the interstitium has been shown to participate in the fluid and electrolyte exchange as well as endocrine functions of the kidney.

Adenine phosphoribosyltransferase deficiency is a rare autosomal recessive metabolic disorder caused by mutations of the APRT gene. Adenine phosphoribosyltransferase (APRT) catalyzes the creation of pyrophosphate and adenosine monophosphate from 5-phosphoribosyl-1-pyrophosphate and adenine. Adenine phosphoribosyltransferase is a purine salvage enzyme. Genetic mutations of adenine phosphoribosyltransferase make large amounts of 2,8-Dihydroxyadenine causing urolithiasis and renal failure.
Phosphate nephropathy or nephrocalcinosis is an adverse renal condition that arises with a formation of phosphate crystals within the kidney's tubules. This renal insufficiency is associated with the use of oral sodium phosphate (OSP) such as C.B. Fleet's Phospho soda and Salix's Visocol, for bowel cleansing prior to a colonoscopy.

Balkan endemic nephropathy (BEN) is a form of interstitial nephritis causing kidney failure. It was first identified in the 1920s among several small, discrete communities along the Danube River and its major tributaries, in the modern countries of Croatia, Bosnia and Herzegovina, Serbia, Kosovo, Romania, and Bulgaria. It is caused by small long-term doses of aristolochic acid in the diet. The disease primarily affects people 30 to 60 years of age. Doses of the toxin are usually low and people moving to endemic areas typically develop the condition only when they have lived there for 10–20 years. People taking higher doses of aristolochic acid have developed kidney failure after shorter durations of exposure.

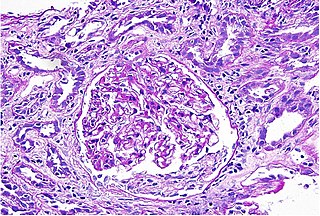
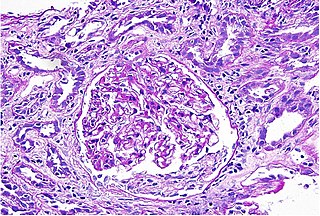
Mesangial proliferative glomerulonephritis (MesPGN) is a morphological pattern characterized by a numerical increase in mesangial cells and expansion of the extracellular matrix within the mesangium of the glomerulus. The increase in the number of mesangial cells can be diffuse or local and immunoglobulin and/or complement deposition can also occur. MesPGN is associated with a variety of disease processes affecting the glomerulus, though can be idiopathic. The clinical presentation of MesPGN usually consists of hematuria or nephrotic syndrome. Treatment is often consistent with the histologic pattern of and/or disease process contributing to mesangial proliferative glomerulonephritis, and usually involves some form of immunosuppressant.

Polycystic kidney disease is a genetic disorder in which the renal tubules become structurally abnormal, resulting in the development and growth of multiple cysts within the kidney. These cysts may begin to develop in utero, in infancy, in childhood, or in adulthood. Cysts are non-functioning tubules filled with fluid pumped into them, which range in size from microscopic to enormous, crushing adjacent normal tubules and eventually rendering them non-functional as well.
Diffuse proliferative glomerulonephritis (DPGN) is a type of glomerulonephritis that is the most serious form of renal lesions in SLE and is also the most common, occurring in 35% to 60% of patients. In absence of SLE, DPGN pathology looks more like Membranoproliferative glomerulonephritis
Onconephrology is a specialty in nephrology that deals with the study of kidney diseases in cancer patients. A nephrologist who takes care of patients with cancer and kidney disease is called an onconephrologist. This branch of nephrology encompasses nephrotoxicity associated with existing and novel chemotherapeutics, kidney disease as it pertains to stem cell transplant, paraneoplastic kidney disorders, paraproteinemias, electrolyte disorders associated with cancer, and more as discussed below.
Mesoamerican nephropathy (MeN) is an endemic, non-diabetic, non-hypertensive chronic kidney disease (CKD) characterized by reduced glomerular filtration rate (GFR) with mild or no proteinuria and no features of known primary glomerular diseases. MeN is prevalent in agricultural communities along the Pacific Ocean coastal lowlands Mesoamerica, including southern Mexico, Guatemala, El Salvador, Nicaragua, Honduras and Costa Rica. Although most cases have been described among agricultural workers, MeN has also been described in other occupations, including miners, brick manufacturers, and fishermen. A common denominator among these occupations is that they are outdoor workers who reside in rural areas in hot and humid climates.
Chronic kidney disease of unknown etiology (CKDu) is an increasing health concern in Sri Lanka. CKDu is recognized as chronic kidney disease without the usual associated causative factors. The first cases of CKDu were reported in Sri Lanka's North Central Province (NCP). Chronic kidney disease, was identified as the 8th leading cause of in-hospital mortality in Sri Lanka, and the leading cause of death in Anuradhapura and Polonnaruwa in 2016. This rise in mortality coincided with the increasing cases of CKDu seen across the country. Studies have shown an estimated 70,000 CKDu patients in high risk areas. Various possible causes for CKDu in Sri Lankans have been investigated, including poisoning from metals, cyanobacteria toxins, agrochemicals, and heat stress, but no definite causes have been identified.
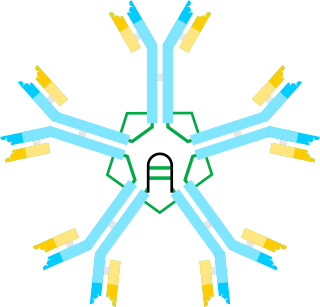
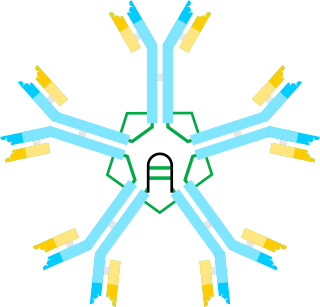
IgM nephropathy or immunoglobulin M nephropathy (IgMN) is a kind of idiopathic glomerulonephritis that is marked by IgM diffuse deposits in the glomerular mesangium. IgM nephropathy was initially documented in 1978 by two separate teams of researchers.